INTRODUCTION
Defination
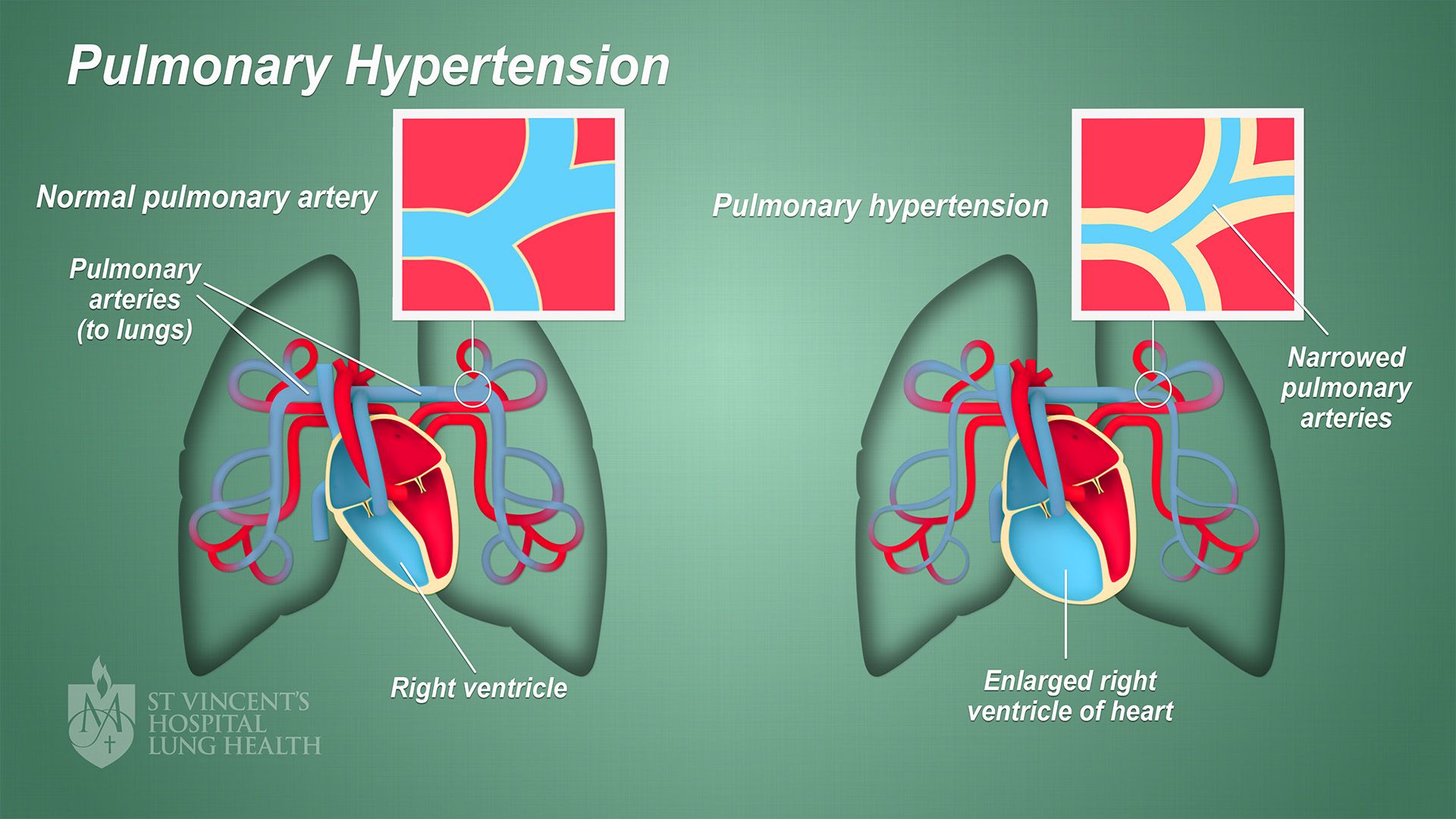
Pulmonary hypertension is increased blood pressure in the arteries of the lungs. and which can be caused by certain drugs like heroin or other intravenous drugs. Over time, it can result in cardiac failure.
Drugs Involved
Heroin, amphetamines, and other substances that affect the pulmonary system.
These conditions highlight the severe risks drug use can have on cardiovascular health. and the importance of seeking help for both addiction and its related health effects. The symptoms of the disease can vary widely. but often include shortness of breath, fatigue, dizziness, chest pain, and swelling in the ankles or legs. As the condition progresses, individuals may experience worsening fatigue, reduced exercise capacity, and signs of heart failure.
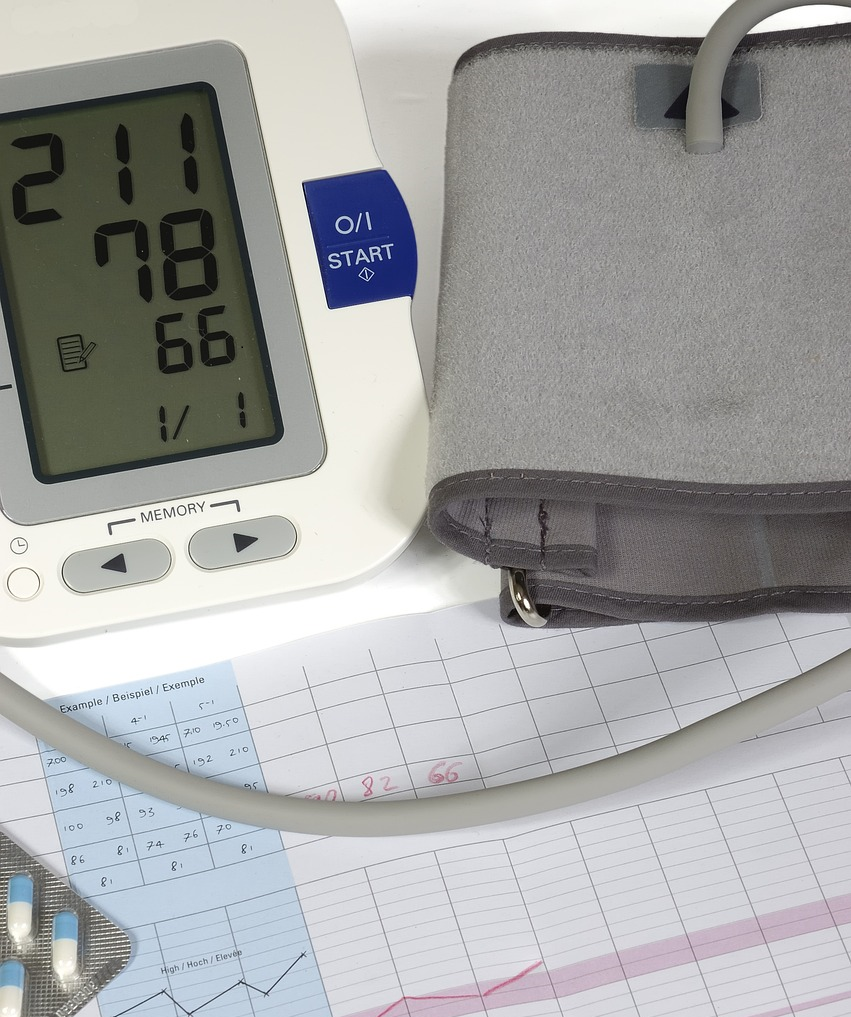
Diagnosis of PH typically involves a combination of clinical evaluation, imaging techniques such as echocardiography. and right heart catheterization, which measures the pressure in the pulmonary arteries. Other tests may be required to determine the underlying cause of the condition.
OVERVIEW
While there is no cure for these disease, treatment focuses on managing symptoms, slowing disease progression. and improving quality of life. Therapeutic options include medications like endothelin receptor antagonists, phosphodiesterase type 5 inhibitors. and prostacyclin analogs, which help relax and widen the pulmonary arteries. In some cases, oxygen therapy, anticoagulants, or even lung transplantation may be considered.
Pulmonary hypertension is a challenging disease with a complex pathophysiology, and early detection is crucial for improving outcomes. Patients diagnosed with PH often require a multidisciplinary approach, including specialized cardiologists, pulmonologists. and other healthcare providers, to manage the condition effectively. Despite difficulties associated with pulmonary hypertension, advances in treatment and management have significantly improved prognosis for many individuals.
PULMONARY HYPERTENSION DUE TO DRUG ADDICTION
HOW DRUG ADDICTION LEADS TO PULMONARY HYPERTENSION
Several medicines, particularly those misused by injection or inhalation, negatively affect the cardiovascular and pulmonary systems, leading to the development of pulmonary hypertension. Drug addiction causes pulmonary hypertension (PH) by directly damaging the pulmonary arteries and increasing resistance to blood flow in the lungs. Stimulants like methamphetamine and cocaine are especially associated with PH, as they cause vasoconstriction (narrowing of blood vessels) and increase blood pressure within the pulmonary arteries. This strains the right side of the heart, which has to work harder to pump blood through the lungs.
Certain drugs, such as opioids, also contribute to PH by impairing the respiratory system. Opioids depress breathing, leading to hypoxia (low oxygen levels), which causes the pulmonary blood vessels to constrict in an attempt to redirect blood flow to areas of the lungs with more oxygen. This raises pressure in the pulmonary arteries and can eventually lead to PH.
Additionally, chronic drug use damages the endothelial cells lining the blood vessels, promotes inflammation, and causes fibrosis (scarring), which further narrows the pulmonary arteries and worsens the condition. Over time, this sustained increase in pressure leads to right heart failure. In summary, drug addiction induces a series of harmful effects, including vasoconstriction, hypoxia, and vascular damage, all of which contribute to the development of the disease. Drugs contribute to PH through several methods, including:
Direct Vasoconstricion (Narrowing of Blood Vessels) :
Some medications constrict blood vessels in the lungs, increasing resistance to blood flow and raising pulmonary artery pressure. This process occurs when some stimulants, such as cocaine and amphetamines, are used. Chronic drug use, particularly injections, can cause inflammation and scarring of pulmonary blood vessels. This injury can reduce blood flow and increase pressure within the pulmonary arteries.
Hypoxia (Low Oxygen Levels) :
Opioids, such as heroin or fentanyl, can cause respiratory depression and decreased oxygen levels in the blood. Chronic low oxygen levels (hypoxia) can cause changes in the pulmonary vasculature, including thickening and narrowing of the arteries, which contribute to the development of disease. Drugs like cocaine and ecstasy (MDMA) can cause endothelial dysfunction, which damages the blood vessel lining. The endothelium controls vascular tone and blood pressure. Damage to this layer can cause pulmonary arteries to contract, increasing pressure in the lungs.
Infection-Related Causes:
Using infected needles or sharing them can introduce germs into the bloodstream, resulting in illnesses including infective endocarditis. These infections can travel to the lungs, producing inflammation and damage to the pulmonary vascular, perhaps leading to the development of pulmonary hypertension.
DRUGS COMMONLY ASSOCIATED WITH PULMONARY HYPERTENSION
Pulmonary hypertension (PH) can be caused or exacerbated by certain drugs. Here are some common drugs associated with pulmonary hypertension:
1.Appetite suppressants (anorexigenic drugs):
Fen-Phen (Fenfluramine and Phentermine): These were once popular weight-loss drugs, but they have been linked to pulmonary hypertension, specifically a condition called pulmonary arterial hypertension (PAH).
2.Amphetamines and related stimulants:
Methamphetamine and Ecstasy (MDMA): These can contribute to the development of PH, especially with chronic use.
Cocaine: Cocaine use can lead to the development of pulmonary hypertension due to its vasoconstrictive effects on the pulmonary arteries.
3.Certain chemotherapy agents:
Mitomycin-C, Bleomycin, and other chemotherapeutic drugs can damage the lung tissue, leading to pulmonary hypertension over time.
4.Nonsteroidal anti-inflammatory drugs (NSAIDs):
Long-term use of NSAIDs may exacerbate PH in some patients, though the mechanism is not fully understood.
Interferon therapy: Used for certain viral infections or cancers, interferon can cause pulmonary hypertension, though this is relatively rare.
Sildenafil (when used inappropriately): While sildenafil (Viagra) is used to treat pulmonary hypertension in appropriate doses, in some cases or when abused in higher doses, it may have harmful effects on pulmonary vascular tone.
If you’re dealing with pulmonary hypertension or concerned about the effects of a specific medication, it’s important to consult a healthcare provider to understand the risks and potential management options.
SIGN & SYMPTOMS OF PULMONARY HYPERTENSION
Pulmonary hypertension (PH) often develops slowly, and its symptoms may be mild at first, making it difficult to diagnose in its early stages. As the condition progresses, however, the symptoms become more pronounced and can significantly impact a person’s quality of life. Common signs and symptoms of pulmonary hypertension include:
- Shortness of Breath (Dyspnea): One of the earliest and most common symptoms, especially during physical activity or exertion. As PH worsens, shortness of breath can occur even at rest.
- Fatigue: Due to the heart’s increased workload in response to elevated pulmonary pressure, patients may feel tired or weak, even after minimal exertion.
- Chest Pain or Discomfort: The increased strain on the heart can lead to chest pain or a feeling of pressure, often described as discomfort or tightness in the chest.
- Swelling (Edema): Fluid retention can cause swelling in the lower legs, ankles, and abdomen. This is often a sign that the right side of the heart is struggling to pump blood effectively, leading to right heart failure.
- Dizziness or Fainting (Syncope): In more advanced cases, reduced blood flow and oxygen supply to the brain may cause lightheadedness, dizziness, or even fainting spells.
- Palpitations: An irregular or rapid heartbeat may occur as the heart attempts to compensate for the increased workload.
- Cyanosis: In severe cases, a bluish tint may develop in the lips, skin, or nails due to low oxygen levels in the blood (hypoxemia).
These symptoms may worsen over time and significantly affect daily activities. Early detection and treatment are important to manage pulmonary hypertension and prevent complications.
TYPES OF PULMONARY HYPERTENSION :-
The World Health Organization (WHO) categorizes pulmonary hypertension into five classes:
1. Pulmonary Arterial Hypertension (PAH) – Group 1
Description: Pulmonary Arterial Hypertension (PAH) refers to high blood pressure in the small arteries of the lungs. It can be caused by a variety of factors, including genetic predisposition, drug use, and other diseases.
- Causes:
- Idiopathic (unknown cause)
- Heritable (genetic mutations, such as BMPR2 gene mutations)
- Drug-induced (e.g., stimulants like cocaine, certain chemotherapy drugs, anorexigenic drugs like fenfluramine)
- Associated with other conditions like HIV, scleroderma, portal hypertension, and congenital heart defects
- Pulmonary veno-occlusive disease (PVOD)
- Symptoms: Shortness of breath, fatigue, chest pain, dizziness, and fainting.
- Treatment: Includes vasodilators (e.g., prostacyclin analogs, endothelin receptor antagonists), oxygen therapy, and sometimes lung transplants.
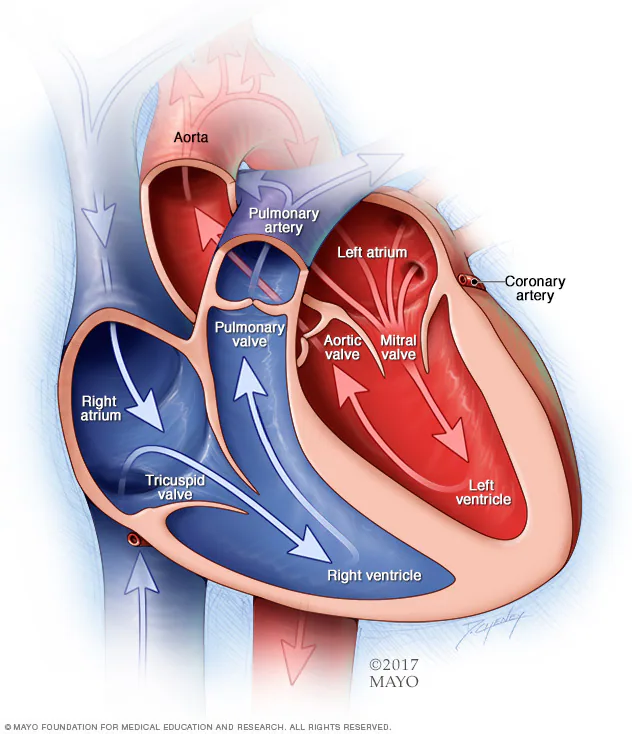
2. Pulmonary Hypertension Due to Left Heart Disease – Group 2
Description: This type of pulmonary hypertension results from left-sided heart conditions that increase pressure in the lungs, including diseases that affect the left ventricle, left atrium, and heart valves.
- Causes:
- Left-sided heart failure (congestive heart failure)
- Valvular heart disease (e.g., mitral or aortic valve disease)
- Congenital heart defects like atrial septal defects
- Symptoms: Similar to those of heart failure, including shortness of breath, fatigue, and swelling in the lower legs and abdomen.
- Treatment: Focuses on managing the underlying heart condition, such as heart failure medications, diuretics, and valve replacement or repair if necessary.
3. Pulmonary Hypertension Due to Lung Disease and Hypoxia – Group 3
Description: This type occurs due to chronic lung diseases or conditions that impair oxygen levels in the blood, leading to increased pressure in the pulmonary arteries.
- Causes:
- Chronic obstructive pulmonary disease (COPD)
- Interstitial lung diseases (e.g., pulmonary fibrosis)
- Obstructive sleep apnea or other sleep-disordered breathing
- Chronic hypoxia (e.g., due to living at high altitudes)
- Symptoms: Shortness of breath, fatigue, and symptoms of the underlying lung disease (e.g., cough, wheezing).
- Treatment: Managing the underlying lung disease, oxygen therapy, pulmonary rehabilitation, and sometimes medications to relieve pulmonary pressure.
4. Chronic Thromboembolic Pulmonary Hypertension (CTEPH) – Group 4
Description: This form of pulmonary hypertension is caused by the chronic blockage or scarring of the pulmonary arteries due to blood clots (pulmonary embolism). If a person has recurrent or unresolved pulmonary embolism, it can lead to permanent damage to the pulmonary vessels, resulting in pulmonary hypertension.
- Causes:
- Chronic pulmonary embolism (blood clots in the lungs)
- Recurrent clots that cause persistent obstruction and increase pulmonary artery pressure.
- Symptoms: Shortness of breath, chest pain, fatigue, and sometimes symptoms of deep vein thrombosis (DVT) or embolism.
- Treatment: Anticoagulants, surgical options (e.g., pulmonary thromboendarterectomy), and in some cases, a lung transplant or pulmonary vasodilators.
5. Pulmonary Hypertension with Unclear or Multifactorial Mechanisms – Group 5
Description: This category includes pulmonary hypertension that doesn’t fit neatly into the other groups and is caused by a combination of factors or unclear mechanisms.
- Causes:
- Hematologic disorders (e.g., sickle cell disease, chronic anemia)
- Metabolic disorders (e.g., thyroid disease, Gaucher’s disease)
- Systemic disorders (e.g., sarcoidosis, vasculitis)
- Chronic kidney disease or other systemic conditions
- Symptoms: Varies depending on the underlying condition, but typically includes symptoms of pulmonary hypertension like shortness of breath, fatigue, and chest pain.
- Treatment: A tailored approach depending on the specific underlying conditions, which may include medications for blood disorders, immune-modulating drugs, or other therapies specific to the cause.
RISK FACTORS OF PULMONARY HYPERTENSION :-
The risk factors for pulmonary hypertension (PH) can vary depending on the underlying cause of the condition. However, several general risk factors may increase a person’s likelihood of developing pulmonary hypertension:
1.Family History
- Genetic predisposition: A family history of pulmonary hypertension, especially idiopathic pulmonary arterial hypertension (IPAH) or heritable pulmonary arterial hypertension (HPAH), increases the risk. Genetic mutations, such as in the BMPR2 gene, are commonly involved.
2.AGE
- Older adults: Pulmonary hypertension is more commonly seen in older adults, especially those with heart or lung diseases.
- Children: Certain genetic or congenital conditions can lead to PH in childhood, though it’s more rare.
3.UNDERLYING HEALTH CONDITION
- Heart disease: People with left heart disease (heart failure, valve disorders) or congenital heart defects are at higher risk for developing pulmonary hypertension.
- Chronic lung disease: Conditions like chronic obstructive pulmonary disease (COPD), interstitial lung disease (ILD), and pulmonary fibrosis can lead to PH due to long-term oxygen deficiency and damage to lung tissue.
- Sleep apnea: Obstructive sleep apnea can lead to low oxygen levels during sleep, which can eventually cause PH.
- Obesity: Severe obesity or obesity hypoventilation syndrome can lead to PH due to low oxygen levels and increased strain on the heart and lungs.
4.CHRONIC BLOOD CLOTS(CTEPH)
- Previous pulmonary embolism (PE): Individuals who have experienced pulmonary embolism (blood clots in the lungs) may develop chronic thromboembolic pulmonary hypertension (CTEPH), where the blood clots cause long-term obstruction and high pulmonary pressures.
5.CONNECTIVE TISSUE DISEASE
- Autoimmune or inflammatory disorders: Conditions like scleroderma (systemic sclerosis), lupus, rheumatoid arthritis, and dermatomyositis can lead to pulmonary hypertension due to vascular damage in the lungs.
6.INFECTIONS
- HIV infection: People with HIV have an increased risk of developing pulmonary hypertension due to vascular changes associated with the infection.
- Schistosomiasis: Parasitic infections (mainly in developing countries) can lead to pulmonary hypertension by affecting the pulmonary arteries.
7.LIVER DISEASE
- Portal hypertension: Cirrhosis or other chronic liver diseases can lead to portal hypertension (elevated blood pressure in the liver), which can cause pulmonary hypertension, a condition called portopulmonary hypertension.
8.DRUGS AND TOXINS
- Certain medications: Some drugs, such as appetite suppressants (e.g., fenfluramine) or certain chemotherapy agents, can increase the risk of pulmonary hypertension.
- Illicit drug use: Drugs like cocaine and methamphetamine can also contribute to PH due to their effects on the blood vessels.
9.PREGNANCY
- Pregnancy-related PH: Pulmonary hypertension can sometimes worsen during pregnancy or cause complications, especially in women with pre-existing PH.
10.BLOOD DISORDERS
- Polycythemia: An overproduction of red blood cells can increase blood viscosity and contribute to increased pressure in the pulmonary arteries.
- Sickle cell disease: This blood disorder can lead to pulmonary hypertension due to repeated blood clots or chronic lung damage.
11.ENVIRONMENTAL & OCCUPATIONAL EXPOSURE
- High-altitude living: Prolonged exposure to low oxygen levels at high altitudes may increase the risk of developing PH.
- Exposure to toxins or chemicals: Certain workplace exposures, such as asbestos or silica dust, can increase the risk of pulmonary hypertension.
12.SMOKING
- Cigarette smoking: Smoking damages the lungs and blood vessels, which can increase the risk of developing PH, especially in combination with other conditions like COPD.
13.OTHER RARE CONDITION
- Sarcoidosis: This inflammatory disease can cause pulmonary hypertension if it affects the lungs and pulmonary arteries.
- Neurofibromatosis: A genetic disorder that can lead to vascular changes and contribute to PH.
14.UNEXPLAINED OR IDIOPATHIC FACTORS
- In some cases, no clear cause for pulmonary hypertension can be identified, and the condition is classified as idiopathic pulmonary hypertension.
WHAT IS THE FIRST AID FOR PULMONARY HYPERTENSION ?
Pulmonary hypertension (PH) is a serious condition characterized by high blood pressure in the arteries of the lungs, which can lead to heart failure and other complications. While pulmonary hypertension typically requires long-term management by healthcare professionals, there are certain first aid measures that can help manage symptoms during an emergency.
1.Stay Calm and Keep the Person Calm
-
- Reassurance: Help the person stay calm to avoid an increase in heart rate or blood pressure. Anxiety and stress can worsen symptoms of pulmonary hypertension.
- Breathing Control: Encourage slow, deep breaths to help the person manage shortness of breath. This can help reduce anxiety and improve oxygenation.
2.Positioning the Person
-
- Sit Them Upright: If the person is experiencing shortness of breath or light headedness, help them sit upright with their legs dangling or slightly elevated. This position helps reduce the pressure on the heart and lungs.
- Avoid Lying Down: Lying down may make breathing more difficult for someone with pulmonary hypertension, as it can increase pressure on the heart and lungs.
3.Administer Oxygen (if prescribed)
-
- Oxygen Therapy: If the person has been prescribed supplemental oxygen due to their pulmonary hypertension, administer it as directed. This can help improve oxygen levels in the blood and ease breathing difficulties.
- Monitor Oxygen Saturation: If available, use a pulse oximeter to check their oxygen saturation levels. If it drops significantly (below 90%), emergency medical help may be needed.
4.Medication Administration (if applicable)
-
- Nitric Oxide or Other Medications: Some people with pulmonary hypertension are prescribed medications like nitric oxide or prostacyclin to help relax the pulmonary arteries and improve blood flow. If they carry any medication, like an inhaler or nebulizer, assist them in taking it as directed.
- Diuretics: If the person is on diuretics to manage fluid buildup, help them take the prescribed dose if it’s due.
5.Monitor for Signs of Worsening Symptoms
-
- Worsening Symptoms: Be vigilant for signs of worsening symptoms, such as increasing shortness of breath, chest pain, fainting, swelling in the legs or abdomen, or confusion. These may indicate that the condition is deteriorating and require immediate medical intervention.
6.Call Emergency Medical Help
-
- Dial Emergency Services: If the person experiences severe symptoms, such as sudden chest pain, severe shortness of breath, dizziness, or loss of consciousness, call emergency services immediately. Pulmonary hypertension can lead to life-threatening complications like right-sided heart failure or pulmonary embolism.
- Provide Medical History: When emergency services arrive, provide them with details about the person’s medical history, current medications, and symptoms to assist in their care.
HOW CAN NASHA MUKTI KENDRA HELP TO TREAT PULMONARY HYPERTENSION OF DRUGS ADDICTED PATIENT ?
1. Preventing Further Lung Damage
- Addressing substance abuse: Drugs like tobacco (smoking) and certain illegal substances are known to damage the lungs and contribute to the development of pulmonary hypertension. Quitting these substances under professional guidance at a Nasha Mukti Kendra reduces the risk of further damage to lung function, which can help slow down the progression of PH.
- Providing education: Through education, counseling, and support, patients can learn how their drug use affects their lungs and heart. This understanding can be motivating for the patient to stay away from harmful substances, thus reducing the chances of further pulmonary complications.
2. Co-Management of Pulmonary Hypertension
- Medical support: While the Nasha Mukti Kendra itself does not provide specialized treatment for PH, it can collaborate with hospitals or clinics where the patient can receive medical treatment for pulmonary hypertension (e.g., medications like vasodilators, oxygen therapy, etc.).
- Monitoring health: Patients in recovery from drug addiction with PH need ongoing monitoring for signs of PH progression. A Nasha Mukti Kendra can support this by ensuring the patient keeps up with regular medical check-ups and reports symptoms to a healthcare provider.
3. Psychological Support and Counseling
- Mental health support: Addiction often has psychological roots, and drug abuse can worsen conditions like PH due to stress and neglect of one’s health. Psychological counseling and therapies (e.g., cognitive-behavioral therapy) offered in drug rehabilitation centers can help patients manage emotional distress and prevent relapse, promoting overall well-being.
- Addressing dual diagnoses: Many patients with PH who are also drug addicts may suffer from depression, anxiety, or other mental health conditions. The Nasha Mukti Kendra can provide holistic treatment that addresses both the addiction and the psychological aspects of the patient’s health.
CONCLUSION
Pulmonary hypertension is a serious condition that can be caused by a range of diseases and factors. The treatment options vary widely depending on the underlying cause, and may include medications, oxygen therapy, lifestyle modifications, and in some cases, surgical interventions. Early diagnosis and management are key to improving quality of life and prognosis for those affected by pulmonary hypertension. Pulmonary hypertension due to drug addiction is a serious health condition that can arise from the direct and indirect effects of drug use on the pulmonary and cardiovascular systems. The drugs themselves, along with the lifestyle associated with addiction, can cause significant damage to the lung vasculature, leading to elevated pulmonary pressure and subsequent strain on the heart.