WHAT IS BONE MARROW ?
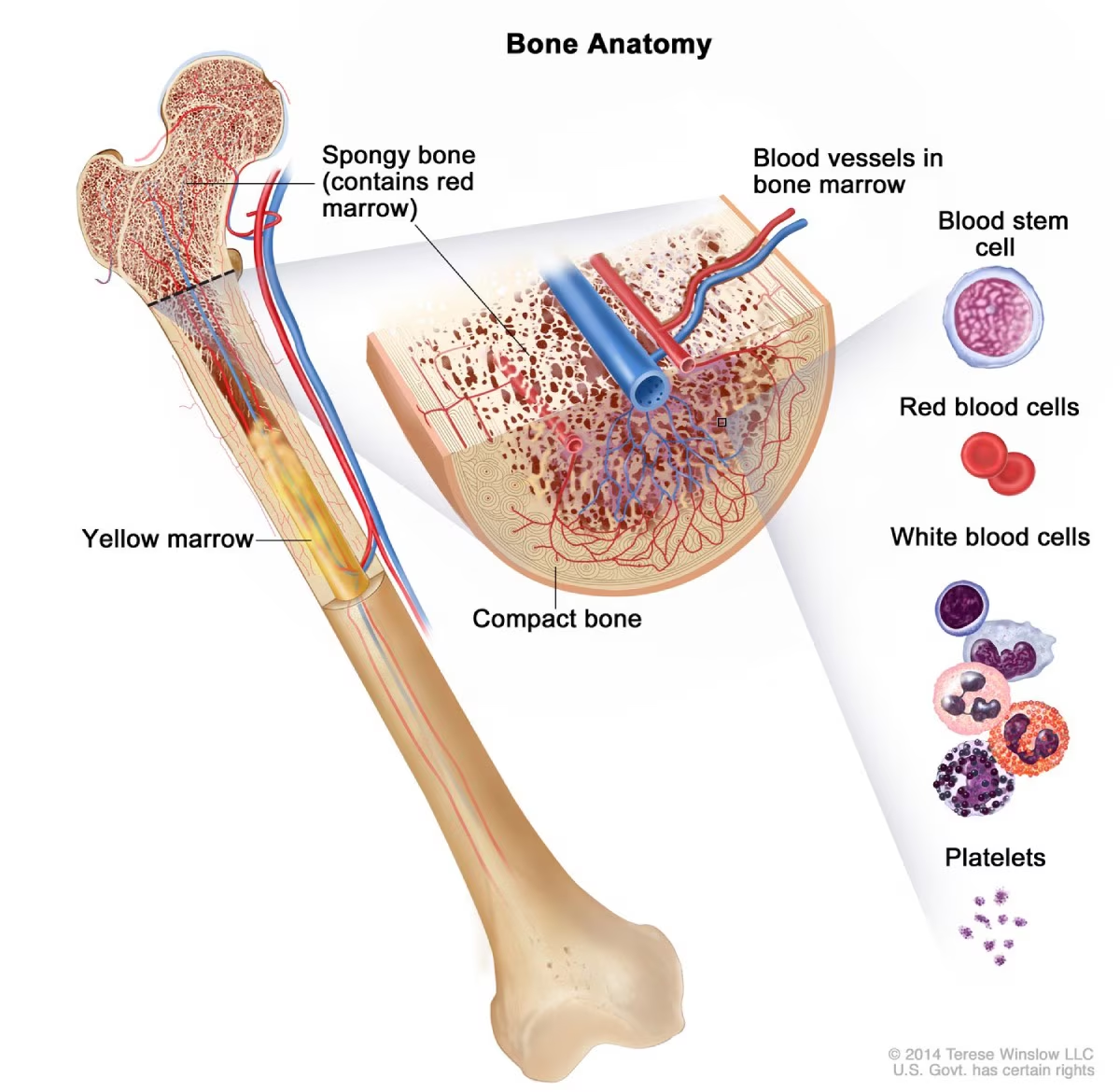
Bone marrow is a soft, spongy tissue found inside certain bones, such as the hip, breastbone, and ribs. It plays an essential role in producing blood cells. This tissue contains specialized cells that create red blood cells, white blood cells, and platelets. Red blood cells transport oxygen throughout the body, white blood cells fight infections, and platelets enable blood clotting and wound healing. Doctors consider Bone Marrow Suppression one of the most dangerous diseases related to bone marrow.
Bone marrow is a key part of the body’s immune system and overall health. It resides in the central cavities of bones and works closely with the circulatory system. The marrow’s ability to produce blood cells continuously is vital for maintaining a balanced and healthy blood supply. When the body faces challenges like blood loss or disease, the marrow adjusts to meet the body’s needs by increasing blood cell production.
Bone marrow disorders can cause serious health issues. For example, doctors diagnose conditions like leukemia, anemia, or aplastic anemia when the marrow doesn’t function properly, producing either too few blood cells or abnormal ones. In such cases, medical treatments like bone marrow transplants may be necessary to restore normal function.
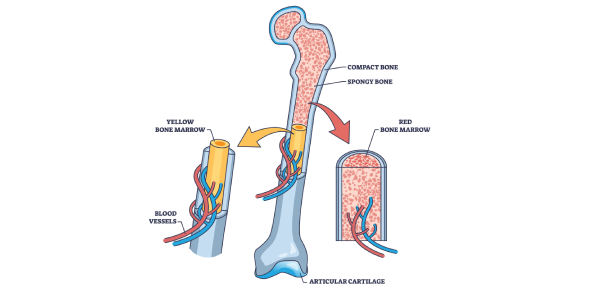
TYPES OF BONE MARROW
There are two types of bone marrow :
- Red marrow
- Yellow marrow
RED BONE MARROW
FUNCTION
Red bone marrow is primarily responsible for producing blood cells. It contains stem cells that develop into three main types of blood cells :
-
- Red blood cells (erythrocytes): Carry oxygen throughout the body.Red blood cells (RBCs), also known as erythrocytes, are the most abundant type of blood cell in the human body.
- White blood cells (leukocytes): White blood cells (WBCs), or leukocytes, are crucial components of the immune system that help defend the body against infections and foreign invaders.
- Platelets (thrombocytes): Help in blood clotting to stop bleeding.Platelets (or thrombocytes) are small, disc-shaped cells involved in blood clotting and wound healing.
LOCATION
Red bone marrow is primarily found in the following locations in the human body:
Flat Bones: These include bones like the sternum (breastbone), ribs, and pelvis.
Long Bones: In the proximal ends of the femur (thigh bone) and humerus (upper arm bone), red marrow is found, particularly in adults. The marrow is more concentrated in the ends (epiphyses) of these bones.
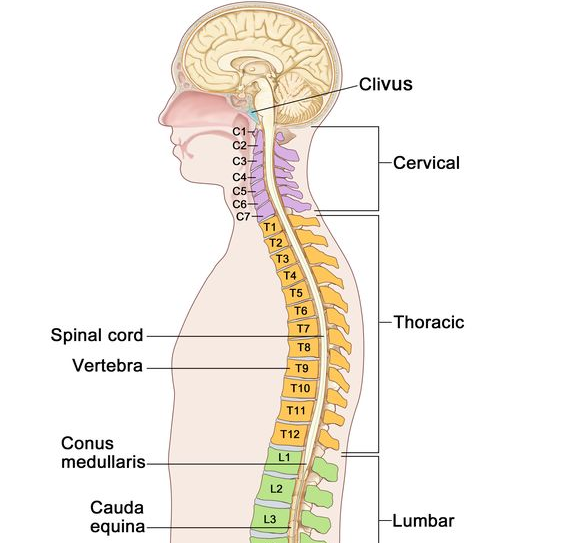
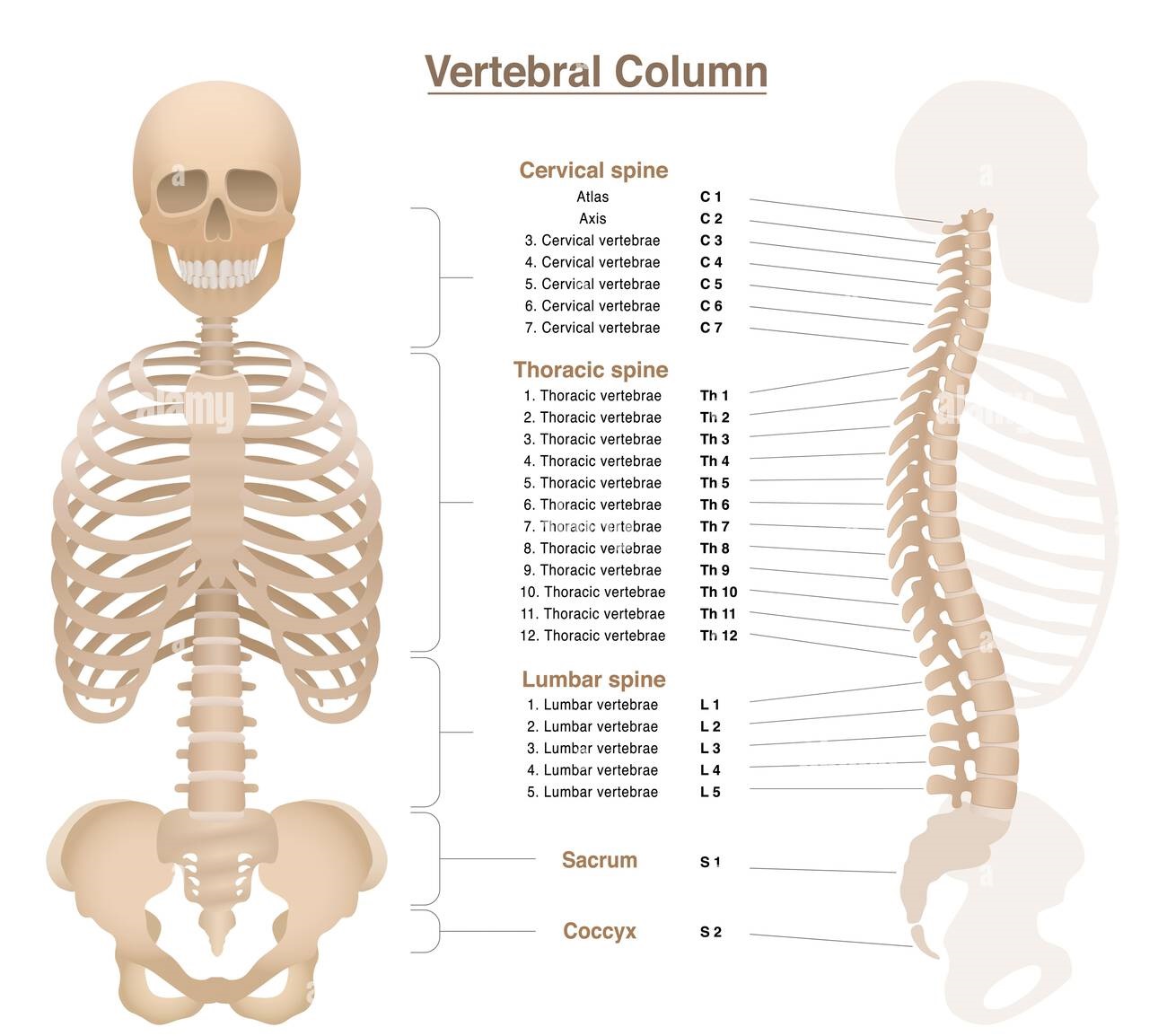
Vertebrae: The bones of the spine also contain red bone marrow.
Skull: The bones of the skull house red marrow.

YELLOW BONE MARROW
FUNCTION
Yellow bone marrow primarily stores fat. It mostly consists of adipocytes (fat cells) and serves as an energy reserve for the body. People find this type of marrow in the central cavities of long bones, such as the femur and humerus. While yellow marrow doesn’t directly produce blood cells under normal conditions, it can convert back to red bone marrow if needed, such as during severe blood loss or when the body requires more blood cells. This adaptability allows the body to maintain blood cell production during critical situations.
Adipocytes (fat cells) in yellow bone marrow are specialized cells that store fat, which serves as an energy reserve for the body. The presence of these fat cells gives yellow marrow its characteristic color.
In certain conditions, such as severe blood loss or anemia, yellow bone marrow converts to red bone marrow. This adaptive response helps the body increase blood cell production when necessary.
LOCATION
Yellow bone marrow is primarily located in the central cavities of long bones. This includes the shafts of bones such as:
- Femur (thigh bone)
- Humerus (upper arm bone)
- Tibia and Fibula (shin bones)
- Radius and Ulna (forearm bones)
In addition, yellow marrow can also be found in the pelvic bones, vertebrae, ribs, and sternum in adults. As we age, much of the red bone marrow is replaced by yellow marrow, which is why it becomes more prominent in adult skeletons.
FUNCTION OF BONE MARROW
Bone marrow is a critical tissue within the body that is involved in several vital functions, primarily related to the production of blood cells and the support of the immune system. Bone marrow is located inside certain bones, such as the ribs, pelvis, skull, and the ends of long bones. Two types of bone marrow—red marrow and yellow marrow—are present, each with specific functions. Below, the key functions of bone marrow are listed:
HEMATOPOIESIS (BLOOD CELL PRODUCTION)
The most important function of bone marrow is the production of blood cells, a process called hematopoiesis. The marrow produces three main types of blood cells:
- Red Blood Cells (Erythrocytes):
- These cells carry oxygen from the lungs to the rest of the body and return carbon dioxide from the tissues to the lungs for exhalation. The production of red blood cells is crucial for maintaining adequate oxygen levels in the body.
- The process of red blood cell production in the marrow is stimulated by a hormone called erythropoietin, which is released by the kidneys when oxygen levels are low.
- White Blood Cells (Leukocytes):
- White blood cells are essential for immune defense. They help the body fight infections by recognizing and attacking harmful pathogens like bacteria, viruses, and fungi.
- There are different types of white blood cells, including neutrophils, lymphocytes, monocytes, eosinophils, and basophils, all of which have specialized roles in the immune system.
- Platelets (Thrombocytes):
- Platelets are involved in blood clotting, helping to stop bleeding by forming clots at the site of injury. They are essential for wound healing and preventing excessive blood loss after injuries.
- Platelet production is regulated by a hormone called thrombopoietin, produced mainly by the liver.
IMMUNE SYSTEM SUPPORT
- Bone marrow is a major site of lymphocyte production, which are a type of white blood cell involved in adaptive immunity. Lymphocytes include T-cells (which help in cell-mediated immunity) and B-cells (which produce antibodies to fight infections).
- Bone marrow also produces granulocytes (such as neutrophils, eosinophils, and basophils) which are part of the body’s innate immune system. These cells play a critical role in responding to infections, particularly bacterial infections.
FAT STORAGE (YELLOW BONE MARROW)
- Yellow bone marrow primarily consists of fat cells and serves as an energy reservoir. When the body faces low energy, yellow marrow can convert back into red marrow to assist with blood cell production, particularly during significant blood loss or when the body needs more red blood cells.
- Though yellow marrow doesn’t directly contribute to blood cell production under normal circumstances, it plays an important role in energy metabolism.
SUPPORT FOR BONE HEALTH
- Bone marrow is located within the bone tissue, and in this way, it plays a role in supporting bone health and structure. The process of hematopoiesis occurs within the trabecular (spongy) bone, which provides a supportive environment for blood cell formation and growth.
- The bone marrow’s interaction with the surrounding bone and bone marrow stroma helps maintain overall skeletal health and integrity.
STORAGE OF STEM CELLS
- Bone marrow contains hematopoietic stem cells—specialized cells capable of dividing and differentiating into all types of blood cells. These stem cells ensure the replenishment of blood cells throughout a person’s life.
- In addition to hematopoietic stem cells, bone marrow also stores mesenchymal stem cells, which can develop into various types of cells, including bone, fat, cartilage, and muscle cells.
- The bone marrow maintains a reserve pool of hematopoietic stem cells. This reserve plays a crucial role, especially during times of stress, such as after blood loss, infection, or chemotherapy.
REGULATION OF BLOOD CELL PRODUCTION
- Bone marrow produces blood cells according to the body’s needs. The production of red blood cells, white blood cells, and platelets is regulated by various signals from the body:
- Erythropoietin (for red blood cells)
- Thrombopoietin (for platelets)
- Various interleukins and growth factors (for white blood cells)
- This regulation ensures that the bone marrow maintains appropriate levels of each type of blood cell, responding to factors such as infection, blood loss, or oxygen levels.
DETOXIFICATION
- Bone marrow can assist in detoxifying the blood by removing toxins or damaged cells. The bone marrow filters out worn-out or damaged blood cells and releases them into the bloodstream for eventual removal by the liver or spleen.
IMPORTANCE OF BONE MARROW
Bone marrow is one of the most critical organs in the body, serving multiple functions that are essential for overall health and survival. Its importance stems from its central role in blood cell production, immune system function, and overall bodily maintenance. Below are the key reasons why bone marrow is so important:
BLOOD CELL PRODUCTION (HEMATOPOIESIS)
The most critical function of bone marrow is the production of blood cells, a process called hematopoiesis. Three different kinds of blood cells are produced by bone marrow:
- Red Blood Cells (Erythrocytes):
- Red blood cells are responsible for carrying oxygen from the lungs to tissues and organs throughout the body. They also help remove carbon dioxide, a waste product, from tissues and transport it back to the lungs for exhalation.
- Without enough red blood cells, the body cannot get enough oxygen, leading to fatigue, weakness, and other symptoms of anemia.
- White Blood Cells (Leukocytes):
- White blood cells are vital components of the immune system. They protect the body from infections, bacteria, viruses, fungi, and abnormal cells, including cancerous cells.
- There are several types of white blood cells, such as neutrophils, lymphocytes, monocytes, basophils, and eosinophils, each with specific roles in defending the body against various threats.
- A deficiency in white blood cells, known as leukopenia, can leave the body vulnerable to infections.
- Platelets (Thrombocytes):
- Platelets are crucial for blood clotting and wound healing. When the skin or blood vessels are injured, platelets form clots to stop bleeding, preventing excessive blood loss.
- A shortage of platelets, or thrombocytopenia, can lead to easy bruising, excessive bleeding, and difficulty stopping bleeding from even minor cuts.
IMMUNE SYSTEM SUPPORT
Bone marrow plays a central role in the body’s immune defense. It produces lymphocytes, a type of white blood cell that is integral to immune responses:
- T-cells: Help fight infections by killing infected cells and coordinating the immune response.
- B-cells: Produce antibodies, proteins that bind to and neutralize harmful pathogens like bacteria and viruses.
- Bone marrow also produces granulocytes, which help fight infections and respond to inflammation and allergens.
A strong immune system, supported by bone marrow, is essential for preventing infections and fighting diseases like cancer, autoimmune disorders, and chronic illnesses.
STORAGE OF STEM CELLS
- Bone marrow stores hematopoietic stem cells, which are undifferentiated cells capable of developing into any type of blood cell. These stem cells are critical for continuously renewing blood cells throughout a person’s life.
- Hematopoietic stem cells differentiate into red blood cells, white blood cells, and platelets, replenishing blood cells as they age or become damaged. Bone marrow also stores mesenchymal stem cells, which can develop into various other cell types, including bone, fat, and cartilage cells.
DETOXIFICATION AND REMOVAL OF WASTE
Bone marrow helps detoxify the blood by removing damaged or old cells, including red blood cells and platelets, which the spleen breaks down. This process maintains the balance of blood cells and prevents the buildup of waste products in the body.
REGENERATION IN RESPONSE TO INJURY OR ILLNESS
Bone marrow can respond to bodily stress by increasing the production of blood cells. For example:
- If there is an acute blood loss due to injury or surgery, the bone marrow increases red blood cell and platelet production to replenish lost blood.
- In cases of infection or immune deficiency, the bone marrow ramps up the production of white blood cells to fight off pathogens.
In extreme cases, if the bone marrow is damaged or not functioning properly, bone marrow transplants or stem cell therapy may be used to restore normal blood cell production.
REGULATION OF BLOOD CELL PRODUCTION
Bone marrow has a sophisticated system for regulating blood cell production, adapting to the body’s needs:
- When there is a drop in oxygen levels, the kidneys release erythropoietin, which signals the bone marrow to produce more red blood cells.
- If there is an infection, the bone marrow will increase production of white blood cells to combat pathogens.
- If the body experiences blood loss or injury, the bone marrow responds by increasing platelet production to aid in clotting and healing.
This self-regulating function ensures that the body always has the right amount of blood cells for healthy functioning.
FAT STORAGE (YELLOW BONE MARROW)
Bone marrow contains yellow marrow, which is mostly composed of fat cells. While yellow marrow doesn’t contribute to blood cell production under normal circumstances, it serves as an energy reservoir. In cases of severe blood loss or when the body needs more blood cells, yellow marrow can convert back to red marrow to assist in blood cell production.
SUPPORT FOR BONE HEALTH
Bone marrow is primarily known for blood cell production, but it also resides within the bones, particularly in the trabecular (spongy) bone. This location provides a strong, protected environment that allows the bone marrow to function effectively. The bone marrow and surrounding bone structures work together to maintain bone health and integrity.
PLATELET PRODUCTION
DISEASE CONDITION : BONE MARROW SUPPRESSION
INTRODUCTION TO BONE MARROW SUPPRESSION
Bone marrow suppression is a condition in which the bone marrow’s ability to make blood cells is decreased or compromised. The bone marrow, located in the middle of the bones, produces three types of blood cells: red blood cells (which transport oxygen), white blood cells (which fight infections), and platelets (which aid in blood clotting). Bone marrow suppression can cause shortages in one or more of these blood components, resulting in a variety of health concerns.
A variety of factors can contribute to this syndrome, including some medications (such as chemotherapy treatments, alcohol, and opioids), infections, autoimmune diseases, and even radiation exposure. In drug addiction, substances such as alcohol, opioids, and other illicit drugs can contribute to bone marrow suppression by either directly damaging the bone marrow or producing nutritional deficits that decrease blood cell production.
Bone marrow suppression symptoms may include weariness, increased susceptibility to infections, easy bruising, and heavy bleeding. The severity of the illness is determined by the degree to which blood cell synthesis is compromised.
Addressing the underlying cause of bone marrow suppression, such as stopping harmful substances or medications, managing infections, and maybe employing medications or therapies to boost blood cell production, is essential for effective treatment. Early detection and intervention are critical for avoiding serious problems while also improving the individual’s general health and quality of life.
CAUSES OF BONE MARROW SUPPRESSION
Bone marrow suppression occurs when the bone marrow’s ability to make blood cells is impaired, resulting in a lack of red blood cells, white blood cells, and platelets. This can lead to anemia, increased susceptibility to infections, and issues with blood coagulation. There are various causes of bone marrow suppression, including medicinal therapies, specific disorders, and lifestyle factors. Some common causes are:
CAUSE OF BONE MARROW SUPRRESSION MEDICATIONS AND TREATMENTS
- Chemotherapy: Chemotherapy drugs used to treat cancer can target rapidly dividing cells, including those in the bone marrow. This often leads to reduced production of blood cells, a common side effect of cancer treatment.
- Radiation Therapy: Radiation, especially when targeted at large areas of the body or the bone marrow, can damage the marrow and impair blood cell production.
- Antibiotics: Certain antibiotics, such as chloramphenicol, can suppress bone marrow function.
- Immunosuppressive Drugs: Medications used to suppress the immune system (such as those used for organ transplants or autoimmune diseases) can affect the bone marrow.
- Anticonvulsants and Antidepressants: Some anticonvulsants and antidepressants, like phenytoin or valproic acid, can cause bone marrow suppression as a side effect.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Long-term use of NSAIDs like ibuprofen or aspirin may cause mild suppression of blood cell production in some individuals.
INFECTIONS RELATED TO BONE MARROW SUPPRESSION
- Viral Infections: Certain viral infections, including human immunodeficiency virus (HIV), hepatitis, and parvovirus, can infect the bone marrow and impair its function.
- Bacterial Infections: Severe bacterial infections, such as sepsis, can overwhelm the bone marrow and lead to suppression.
- Tuberculosis: The tuberculosis bacterium can sometimes infect the bone marrow, leading to a decrease in blood cell production.
NUTRITIONAL DEFICIENCIES
- Vitamin B12 Deficiency: A lack of vitamin B12, often due to poor diet or absorption issues, can impair red blood cell production, leading to anemia.
- Folate Deficiency: Folate (vitamin B9) is crucial for blood cell production, and a deficiency can result in megaloblastic anemia.
- Iron Deficiency: Although more commonly associated with anemia, a severe lack of iron can also affect the bone marrow’s ability to produce red blood cells.
TOXINS AND CHEMICALS
- Chemicals: Exposure to toxic chemicals like benzene (found in industrial settings, cigarette smoke, and certain cleaning products) can lead to bone marrow suppression.
- Pesticides and Herbicides: Long-term exposure to some pesticides and herbicides may affect bone marrow function.
- Heavy Metals: Exposure to heavy metals like lead or arsenic can damage the bone marrow and lead to blood cell production problems.
ALCOHOL ABUSE
- Chronic Alcohol Consumption: Prolonged alcohol abuse can impair the function of the bone marrow, leading to suppressed blood cell production. It can also lead to nutritional deficiencies, which further contribute to bone marrow suppression.
- Alcohol abuse often involves the use of other substances or medications, some of which can further contribute to bone marrow suppression or toxicity. For example, certain medications prescribed for alcohol withdrawal can affect bone marrow function.
AUTOIMMUNE DISEASES
- Systemic Lupus Erythematosus (SLE): In autoimmune diseases like lupus, the immune system mistakenly attacks the bone marrow, leading to bone marrow suppression and low blood cell counts.
- Rheumatoid Arthritis: Similar to lupus, rheumatoid arthritis can lead to bone marrow problems as the immune system affects different tissues, including the marrow.
BONE MARROW SUPPRESSION & DISORDERS
- Aplastic Anemia: This rare condition occurs when the bone marrow fails to produce enough blood cells, leading to pancytopenia (a deficiency of all types of blood cells). It can be caused by an autoimmune response, toxins, or other factors.
- Leukemia: Leukemia is a cancer of the blood-forming tissues, including the bone marrow. It leads to the uncontrolled growth of abnormal white blood cells, which interferes with normal blood cell production.
- Myelodysplastic Syndromes (MDS): These are a group of disorders caused by poorly formed or dysfunctional blood cells in the bone marrow. People with MDS often have low blood cell counts and increased risk of infections and bleeding.
GENETIC DISORDERS
- Fanconi Anemia: This is a rare inherited disorder that affects the bone marrow and leads to bone marrow failure. It can cause a decrease in blood cell production, leading to anemia, infections, and bleeding.
- Shwachman-Diamond Syndrome: A genetic condition that affects bone marrow function, leading to low blood counts and other symptoms like pancreatic insufficiency.
OTHER CONDITIONS
- Hypothyroidism: Low thyroid hormone levels can lead to a reduction in red blood cell production.
- Liver Disease: Severe liver diseases, such as cirrhosis, can lead to bone marrow suppression due to the liver’s role in producing certain blood-clotting factors.
- Sickle Cell Disease: People with sickle cell disease often experience chronic bone marrow stress due to the increased breakdown of red blood cells, which can impact overall marrow function.
CONSEQUENCES OF BONE MARROW SUPPRESSION
Bone marrow suppression can have major effects since the bone marrow is responsible for creating blood cells, which are required for a range of body activities. Suppressing bone marrow can cause shortages in red blood cells, white blood cells, and platelets. These deficiencies can cause a variety of health problems, depending on the kind of blood cell involved. The following are the primary implications of bone marrow suppression:
ANEMIA (LOW RED BLOOD CELLS)
Red blood cells carry oxygen throughout the body. When the bone marrow fails to produce enough red blood cells, the body may become oxygen-deprived, leading to anemia. This condition affects the function of various organs and tissues, making it difficult for the body to perform everyday tasks.
INCREASED RISK OF BLEEDING AND BRUISING (LOW PLATELETS)
Platelets are responsible for blood clotting. When the bone marrow produces too few platelets, the person risks developing thrombocytopenia, condition that causes excessive bleeding, even from minor injuries. This can lead to spontaneous bleeding and difficulty stopping it, which can be life-threatening in severe cases.
ORGAN DYSFUNCTION DUE TO BONE MARROW SUPPRESSION
With inadequate oxygen delivery (from low red blood cell levels) and an increased risk of infections and bleeding, several organs can begin to function poorly:
-
- Heart: The heart may work harder to compensate for the lack of oxygen, leading to strain and potential complications like heart failure.
- Kidneys: If the body becomes anemic or suffers from severe infections, the kidneys may be impacted, leading to kidney dysfunction or even failure.
- Liver: If bone marrow suppression is caused by liver disease, both liver and bone marrow function may decline simultaneously.
BLEEDING IN INTERNAL ORGANS
In severe cases of bone marrow suppression and thrombocytopenia, bleeding can occur in vital organs such as the brain, gastrointestinal tract, and lungs. This can be life-threatening and requires urgent medical attention.
INCREASED RISK OF DEVELOPING CANCER
- In some cases, bone marrow suppression may be related to or a result of underlying conditions like leukemia or myelodysplastic syndromes. These conditions themselves can lead to abnormal cell growth in the bone marrow and increase the risk of developing blood cancers.
DEVELOPMENT OF BONE MARROW FAILURE
- In severe or untreated cases, bone marrow suppression can lead to bone marrow failure, where the marrow stops producing blood cells entirely. This condition is life-threatening and requires urgent medical treatment, such as bone marrow or stem cell transplantation.
INCREASED SUSCEPTIBILITY TO INFECTIONS (LOW WHITE BLOOD CELLS)
White blood cells are essential for fighting infections. Bone marrow suppression often leads to a condition called leukopenia, where the body has insufficient white blood cells to combat infections. This can leave the individual vulnerable to bacterial, viral, or fungal infections, which may be more severe and harder to treat.
INCREASED RISK OF SEVERE INFECTIONS
In addition to leukopenia, bone marrow suppression can impair the overall functioning of the immune system, making it harder for the body to fight off infections. People with bone marrow suppression are at an increased risk of:
-
- Sepsis: A life-threatening infection that spreads throughout the body.
- Pneumonia: A lung infection that can be fatal if untreated, particularly in people with low white blood cells.
- Urinary tract infections: These infections are more common and severe in people with compromised immune systems.V
FATIGUE AND WEAKNESS
Fatigue is one of the most common and debilitating symptoms of bone marrow suppression, primarily caused by low red blood cells (anemia). When the body doesn’t get enough oxygen, people often feel extremely tired, weak, and unable to perform routine tasks. This significantly reduces a person’s quality of life and ability to engage in normal activities.
CHRONIC HEALTH CONDITIONS
Long-term or severe bone marrow suppression can lead to chronic health problems, including:
-
- Chronic anemia: Persistent fatigue, poor concentration, and weakness.
- Immunodeficiency: Recurrent infections that are hard to treat and can lead to complications.
- Persistent bleeding disorders: Ongoing problems with bleeding that may require regular medical intervention, such as platelet transfusions.
COMPROMISED HEALING AND RECOVERY
Bone marrow suppression can slow down the body’s ability to heal wounds or recover from illness. This is particularly problematic for people who need to undergo surgery or have sustained an injury. With a reduced ability to produce platelets and red blood cells, healing and recovery become slower and more complicated.
- Proper Nutrition: Ensure a balanced diet rich in vitamins and minerals, particularly those that aid in tissue repair.
- Treating Underlying Conditions: Managing chronic conditions like diabetes or cardiovascular disease can help improve healing outcomes.
SIGN & SYMPTOMS OF BONE MARROW SUPPRESSION
Bone marrow suppression occurs when the bone marrow loses its ability to produce blood cells. This reduction or impairment can result in a shortage of red blood cells, white blood cells, and platelets, leading to various symptoms. The specific symptoms depend on which type of blood cell is most affected. Common symptoms of bone marrow suppression include:
I.Fatigue and Weakness
- Cause: A decrease in red blood cells (anemia) reduces the amount of oxygen delivered to tissues and organs.
- Symptoms: Persistent tiredness, weakness, shortness of breath, dizziness, and difficulty performing everyday activities.
II.Frequent infections
- Cause: A decrease in white blood cells (leukopenia or neutropenia) impairs the immune system’s ability to fight off infections.
- Symptoms: Recurrent infections, such as respiratory infections, skin infections, or urinary tract infections, that may be more severe than usual. Fever, chills, and other signs of infection are common.
III.East Bruising & Bleeding
- Cause: A decrease in platelets (thrombocytopenia) affects the blood’s ability to clot properly.
- Symptoms:
- Easy bruising or the appearance of purple or red spots on the skin (petechiae).
- Frequent or prolonged nosebleeds.
- Bleeding gums or excessive bleeding from small cuts or injuries.
- Heavy or prolonged menstrual periods (in females).
IV.Pale Skin
- Cause: Low red blood cells (anemia) can lead to insufficient oxygen being carried throughout the body.
- Symptoms: Paleness of the skin, especially in the face, lips, or nail beds.
V.Shortness of Breath
- Cause: Anemia reduces the oxygen-carrying capacity of the blood.
- Symptoms: Difficulty breathing during physical activity or even at rest, especially with exertion.
VI.Rapid Or Irregular Heartbeat
- Cause: The body compensates for low oxygen levels due to a lack of red blood cells.
- Symptoms: A racing or irregular heartbeat (tachycardia), which can be felt as palpitations.
VII.Mouth Sores or Sore Throat
- Cause: A reduction in white blood cells (especially neutrophils) weakens the body’s defense against infections.
- Symptoms: Painful mouth sores, ulcers, or a sore throat, which can make eating or swallowing difficult.
VIII.Excessive Sweating
- Cause: Infections or inflammation due to a weakened immune system.
- Symptoms: Night sweats or unexplained sweating during the day, especially if accompanied by fever or chills.
IX.Headaches & Dizziness
- Cause: Insufficient red blood cells (anemia) leads to a lack of oxygen in the brain.
- Symptoms: Headaches, lightheadedness, or dizziness, especially when standing up quickly or during physical activity.
X.Pain In The Bones Or Joints
- Cause: When the bone marrow is actively trying to compensate for the lack of blood cells, it can become enlarged, leading to pain or discomfort in the bones.
- Symptoms: Aches or pains in the bones, particularly in areas like the sternum, hips, or thighs.
XI.Cold Hands & Feet
- Cause: Reduced oxygen supply to the extremities due to low red blood cell counts.
- Symptoms: Hands and feet may feel cold or numb, especially in the fingers and toes.
XII.Poor Healing Or Wound Recovery
- Cause: Low platelet counts reduce the blood’s ability to form clots, which slows down the healing process.
- Symptoms: Slow or poor healing of cuts or injuries, and wounds that may continue to bleed longer than expected.
XIII.Unexplained Weight Loss
- Cause: Severe infections or certain underlying conditions causing bone marrow suppression (such as leukemia) can result in weight loss.
- Symptoms: Unintentional weight loss without changes in diet or exercise, often accompanied by other symptoms like fever or fatigue.
HOW DRUG ADDICTION AFFECTS ON BONE MARROW ?
Drug addiction can have a major impact on bone marrow function, resulting in a number of health concerns, notably those connected to blood cell formation. The bone marrow produces the body’s blood cells, which include red blood cells (for oxygen delivery), white blood cells (for immune defense), and platelets (for blood clot formation). When drug addiction impairs the natural functioning of bone marrow, it can lead to major consequences. This is how drug abuse affects bone marrow.
A.Suppression of Blood Cell Production
- Opioids: Chronic use of opioids (like heroin and prescription painkillers) can suppress bone marrow activity, reducing the production of essential blood cells, particularly white blood cells. This leads to an increased susceptibility to infections, anemia (due to low red blood cells), and low platelet count (thrombocytopenia).
- Alcohol: Heavy and prolonged alcohol consumption can lead to bone marrow suppression, decreasing the production of red blood cells, white blood cells, and platelets. This can cause anemia, neutropenia (low white blood cell count), and thrombocytopenia, making the body more vulnerable to infections, bleeding, and fatigue.
B.Toxic Effects Of Drugs
- Certain drugs, particularly illicit ones and some medications used in addiction treatment, can be toxic to bone marrow. For instance, chemotherapy drugs used in cancer treatment may damage bone marrow, and other drugs with toxic effects can suppress marrow function, reducing the production of blood cells.
- Cocaine and other stimulants These substances can constrict blood vessels, potentially limiting blood flow to the bone marrow. This can interfere with the marrow’s ability to produce blood cells, contributing to various blood disorders.
C.Nutritional Deficiencies
- Drug addiction is often associated with poor nutrition, which can further affect bone marrow function. Lack of essential nutrients like folic acid, vitamin B12, and iron, which are critical for blood cell production, can lead to conditions like anemia. A deficiency in these nutrients hampers the production of healthy blood cells in the bone marrow.
D.Increased Risk Of Infections
- Drugs like opioids and alcohol weaken the immune system, which is closely tied to the bone marrow’s role in producing white blood cells. With fewer white blood cells, the body’s ability to fight infections is impaired, leaving individuals more vulnerable to illnesses.
E.Increased Risk Of Bood Disorders
- Chronic drug use, especially over the long term, can lead to more severe blood-related conditions. Leukemia (a form of cancer that affects the bone marrow) and other hematological disorders may be more likely to develop due to genetic damage to the marrow cells caused by drug toxins.
F.Bone Marrow Failure
- In extreme cases, drug addiction can lead to bone marrow failure, a condition in which the marrow is unable to produce enough blood cells to meet the body’s needs. If left untreated, this ailment can be fatal.v
DISORDERS OF BONE MARROW SUPPRESSION
Bone marrow suppression can result from a variety of underlying illnesses or external factors that impair the bone marrow’s ability to produce healthy blood cells. This disorder can lead to low numbers of red blood cells (anemia), white blood cells (leukopenia), and platelets (thrombocytopenia). Severe bone marrow suppression can cause various bone marrow problems, some of which are chronic and require medical intervention. Bone marrow suppression can also cause or be related to various illnesses and ailments, which are listed below:
1.Aplastic Anemia
Aplastic anemia is a rare but serious condition where the bone marrow fails to produce enough blood cells—red blood cells, white blood cells, and platelets. This leads to pancytopenia (a deficiency of all three types of blood cells).
2.Leukemia(Bone Marrow Suppression or Disorder)
Leukemia is a group of cancers that affect the blood and bone marrow, causing the production of abnormal white blood cells that do not function properly. These abnormal cells overcrowd the bone marrow and interfere with normal blood cell production.The Types of Leukemia is :-
Acute Leukemia
Rapid development of immature white blood cells.
Chronic Leukemia
Slower-growing form, where more mature but still dysfunctional white blood cells are produced.
3.Myelodysplastic Syndromes (MDS)
MDS is a group of disorders caused by poorly formed or dysfunctional blood cells in the bone marrow. In MDS, the bone marrow does not make enough healthy blood cells, and the blood cells that are made are often abnormal.
4.Bone Marrow Failure
Bone marrow failure occurs when the bone marrow stops producing an adequate number of blood cells, leading to pancytopenia. This can be caused by a variety of diseases and conditions, including aplastic anemia, leukemia, MDS, and certain genetic disorders.
5.Fanconi Anemia
Fanconi anemia is a rare inherited disorder that leads to bone marrow failure. It results in a reduced production of blood cells and an increased risk of developing leukemia and other cancers.
6.Shwachman-Diamond Syndrome
Shwachman-Diamond syndrome is a rare genetic disorder that affects bone marrow function, leading to bone marrow suppression. It also impacts the pancreas and skeletal system.
7.Hypoplastic Anemia
This is a type of anemia in which the bone marrow produces insufficient numbers of red blood cells, leading to low hemoglobin levels and symptoms of anemia. It can also affect the production of other blood cells (white blood cells and platelets).
8.Pure Red Cell Aplasia (PRCA)
PRCA is a rare disorder in which the bone marrow stops producing red blood cells, leading to anemia, while white blood cell and platelet production may remain unaffected.
9.Chronic Myelomonocytic Leukemia (CMML)
CMML is a type of leukemia that has features of both leukemia and myelodysplastic syndromes. It is characterized by an overproduction of monocytes (a type of white blood cell) and abnormal blood cell development.
10.Secondary Bone Marrow Suppression
Bone marrow suppression can also occur as a secondary condition resulting from external factors such as medications, chemotherapy, radiation therapy, or infections.
DIAGNOSIS OF BONE MARROW SUPPRESSION
Bone marrow suppression is diagnosed using a combination of clinical evaluations, laboratory tests, and imaging studies. Common diagnostic procedures include:
A.Clinical Evaluation
Symptoms such as weariness, pallor, bruises, recurrent infections, and easy bleeding could indicate bone marrow suppression.
It’s important to provide a full history of drugs, radiation exposure, prior chemotherapy, family history, and recent infections/autoimmune illnesses.
B.Blood Tests
The Complete Blood Count (CBC) is the primary test to determine the number of red blood cells (RBCs), white blood cells (WBCs), and platelets. Low levels of any of these may suggest bone marrow suppression.
o Retinal cells count: Measures bone marrow’s ability to make red blood cells.
A peripheral blood smear involves examining a blood sample under a microscope for aberrant cell shapes, sizes, or numbers.
C.Bone Marrow Biopsy and Aspiration
This is the gold standard test. A sample of bone marrow (typically from the iliac crest) is collected and examined to determine the amount and type of blood-forming cells. It aids in detecting disorders such as aplastic anemia, leukemia, and myelodysplastic syndromes.
D.Genetic Testing
For suspected inherited illnesses, such as Fanconi anemia, or particular mutations linked to leukemia or myelodysplastic syndromes.
E.Imaging
X-rays, CT scans, or MRIs may be used to diagnose malignancies or metastases in the bone marrow.
F.Infectious Disease Testing
If bone marrow suppression is considered to be caused by an infection, such as parvovirus B19 or HIV, appropriate testing are conducted.
G.Bone Marrow Culture
If a fungal or bacterial infection is detected in the bone marrow, a culture may be obtained.
TREATMENT OF BONE MARROW SUPPRESSION
Treatment is based on the underlying cause of the suppression and may include the following strategies:
1.Addressing the Underlying Cause
To address drug-related issues, the initial step is to discontinue or replace the offending medication, such as chemotherapy or antibiotics.
To treat infections, use antiviral, antibacterial, or antifungal medications as needed.
2.Supportive Care
Blood transfusions
- Red blood cell transfusions for anemia, platelet transfusions for thrombocytopenia, or white blood cell transfusions for neutropenia (if severe).
Growth factors
- Erythropoietin or G-CSF (Granulocyte Colony-Stimulating Factor) may be given to stimulate RBC and WBC production, respectively.
- Thrombopoietin analogs for low platelet counts.
- Antibiotics and Antifungals: In cases of neutropenia, patients may require prophylactic antibiotics or antifungals to prevent infections.
3.Bone Marrow Stimulants & Immune Modulators
Immunosuppressive therapy: Antithymocyte globulin (ATG) and cyclosporine can be used to treat autoimmune-related bone marrow suppression, such as aplastic anemia.
Steroids may be used to treat autoimmune illnesses like lupus that inhibit bone marrow function.
4.Bone Marrow Transplantation
In extreme situations of unresponsive bone marrow failure, such as aplastic anemia, leukemia, or myelodysplastic syndromes, hematopoietic stem cell transplant (bone marrow transplant) may be the sole treatment option.
5.Treatment for Underlying Conditions
Correcting nutritional deficiencies, such as folate, vitamin B12, or iron, can increase bone marrow function.
Chemotherapy can treat cancer, including leukemia, and restore bone marrow function.
6.Cancer-Related Suppression
If bone marrow suppression is caused by cancer or its treatments, controlling the malignancy with chemotherapy, radiation, or targeted therapies may enhance blood cell production.
7.Plasma Exchange
In rare circumstances, such as thrombotic thrombocytopenic purpura, plasma exchange (plasmapheresis) may be necessary.
8.Patient Education and Monitoring
Patients should have blood cell counts checked on a regular basis so that treatment can be adjusted as needed. Furthermore, people with bone marrow suppression should avoid infections, injuries, and bleeding owing to low blood cell counts.
The treatment strategy is personalized to the patient’s exact diagnosis, level of bone marrow suppression, and overall health. Managing bone marrow suppression necessitates interdisciplinary care from hematologists, oncologists, and infectious disease experts.
DIETARY GUIDELINES FOR BONE MARROW SUPPRESSION
Bone marrow suppression occurs when the bone marrow, which generates blood cells, fails to produce enough healthy blood cells, leading to disorders such as anemia, thrombocytopenia (low platelet count), and leukopenia. Chemotherapy, radiation therapy, certain drugs, infections, or underlying disorders can all contribute to this condition. A proper diet plays a crucial role in maintaining the body during bone marrow suppression and improving overall health.
I.Increase Protein Intake
Protein is necessary for the formation of blood cells, tissue repair, and immune system function.
• Sources include lean meats (chicken, turkey), fish, eggs, beans, lentils, tofu, dairy products (milk, cheese, yogurt), and nuts.
• Aim for 1.2-2 g of protein per kilogram of body weight. A doctor or nutritionist can provide personalized advice.
II.Boost Iron-Rich Foods (for Anemia)
Iron is essential for red blood cell synthesis, and insufficient iron levels can lead to anemia, which is a typical side effect of bone marrow suppression.
• Sources include red meat, chicken, turkey, liver, beans, tofu, fortified cereals, spinach, and other leafy greens.
• Combine iron-rich meals with vitamin C, such as citrus fruits, bell peppers, and broccoli, to improve iron absorption.
III.Folate and Vitamin B12 for Healthy Blood Cells
The synthesis and maturation of red blood cells need folate (vitamin B9) and vitamin B12.
• Folate-rich foods include dark leafy greens, beans, lentils, avocados, oranges, and fortified grains.
• Sources of vitamin B12 include animal-based foods such as meat, fish, dairy products, and eggs. Plant-based diets may require fortified foods or supplements.
IV.Incorporate Vitamin C and Zinc
These nutrients are essential for immunological health and wound healing. Vitamin C also improves iron absorption.
• Vitamin C-rich foods include citrus fruits (oranges and grapefruits), strawberries, kiwi, bell peppers, broccoli, and tomatoes.
• Zinc sources: Meat, shellfish, dairy, seeds, nuts, legumes, and whole grains.
V.Healthy Fats for Immune Support
Healthy fats aid the body’s healing process and are essential for overall cell health.
• Sources include avocados, almonds, seeds, olive oil, and fatty fish (e.g. salmon or mackerel).
• Omega-3 fatty acids found in flaxseed, chia seeds, walnuts, and salmon can reduce inflammation.
VI.Stay Hydrated
Adequate hydration is crucial for blood cell health and good body function, particularly when receiving therapies that may cause dehydration.
• Sources include water, herbal teas, and clear broths.
• Avoid caffeine and sugary drinks.
VII.Limit Processed and High-Salt Foods
Processed and salty foods might raise the risk of infection and aggravate inflammation. It is critical to avoid or limit foods that are highly processed, heavy in sodium, and contain unhealthy fats.
• Prioritize whole, less processed foods. • Select low-sodium products and make fresh meals with whole ingredients.
VIII.Iron and Calcium Considerations
Some bone marrow suppression treatments may have an effect on nutrition absorption. For example, increased iron intake can occasionally interfere with calcium absorption.
- Maintain a balanced intake. Ensure that you are getting enough calcium and iron, but not too much of either, to support absorption. If you’re thinking about using supplements, consult your doctor first.
IX.Foods To Avoid During Neutropenia(Low White Blood Cell Count)
If you also have neutropenia (few white blood cells), which raises your risk of infection, you should avoid foods that may contain hazardous bacteria or pathogens. This includes:
• Raw/undercooked foods Avoid consuming raw meats, seafood, and eggs. Only consume well-cooked foods.
• Use unpasteurized goods. Avoid unpasteurized milk, cheese, and juices.
• To prevent foodborne infections, properly wash and peel fresh fruits and vegetables.
X.Small, Frequent Meals
If your appetite is suppressed owing to medication side effects (such as nausea), try eating small, regular meals throughout the day instead of large meals.
- Take iron supplements if iron shortage is detected.
- Use folate or B12 supplements if deficits are discovered.
- Use multivitamins or individual vitamins/minerals to boost immune function and blood health, as needed.
#Key Takeaways
- Prioritize protein-rich foods, iron, folate, vitamin B12, and vitamin C for healthy blood cell synthesis.
• Prioritize hydration and healthy fats, while avoiding high-salt and processed foods.
• Neutropenic individuals should avoid raw or unpasteurized meals to prevent infection risk.
• Collaborate with a healthcare provider or nutritionist to customize dietary advice for your unique illness and treatment plan.
CONCLUSION
Bone marrow suppression, a dangerous consequence, can occur in both drug-addicted individuals and those receiving certain treatments. It results from a decrease in blood cell formation in the bone marrow, leading to anemia, an increased risk of infection, and bleeding issues. This illness significantly impacts the health and well-being of those affected.