WHAT IS COMMUNICABLE DISEASES ?
Communicable Diseases, often known as infectious diseases, are illnesses that can transfer from one person to another or between animals and people. These diseases are caused by pathogens such as viruses, bacteria, fungi, or parasites. They spread through various routes, including direct contact, respiratory droplets, contaminated food or water, and insect bites. When these infections enter the body, they reproduce and cause a variety of symptoms, which can vary in severity depending on the condition. Communicable diseases are particularly concerning because they can spread rapidly, affecting large populations and potentially leading to outbreaks, epidemics, or pandemics.
The global impact of communicable diseases is substantial, as they cause a high number of deaths and illnesses worldwide, especially in countries with limited healthcare resources. For example, emerging diseases like COVID-19 have had an immediate and widespread effect. Beyond the physical harm to human health, communicable diseases also negatively impact the economy, education systems, and healthcare infrastructure.
Public Health Initiatives
Public health initiatives, such as immunization, hygienic improvements, and health education, can help prevent some communicable diseases. Vaccines, for instance, have saved millions of lives by effectively controlling diseases like smallpox, polio, and measles. Surveillance, early detection, and quick response are also essential in preventing the spread of these diseases. However, novel infections, virus mutations, and limited healthcare access can complicate control efforts.
In addition to the physical burden, communicable diseases can carry a social stigma that impacts individuals’ social and psychological well-being. Those infected may face discrimination or social exclusion, which can make diagnosis and treatment even more challenging. Therefore, managing communicable diseases requires not only limiting the physical spread of infections but also addressing the broader socioeconomic implications.
Finally, public health agencies worldwide are working to prevent the spread of infectious diseases by raising awareness, providing treatment, and developing comprehensive plans. To overcome the ongoing challenges posed by communicable diseases and prevent future outbreaks, international cooperation, research, and the availability of medical resources are essential.
Breakdown of Communicable Diseases:
- Spread: Communicable diseases can be transmitted through various means, such as direct contact, droplets, or contaminated substances.
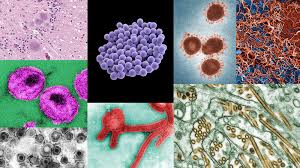
- Cause: They are caused by pathogens—disease-causing microorganisms like viruses, bacteria, fungi, or parasites.
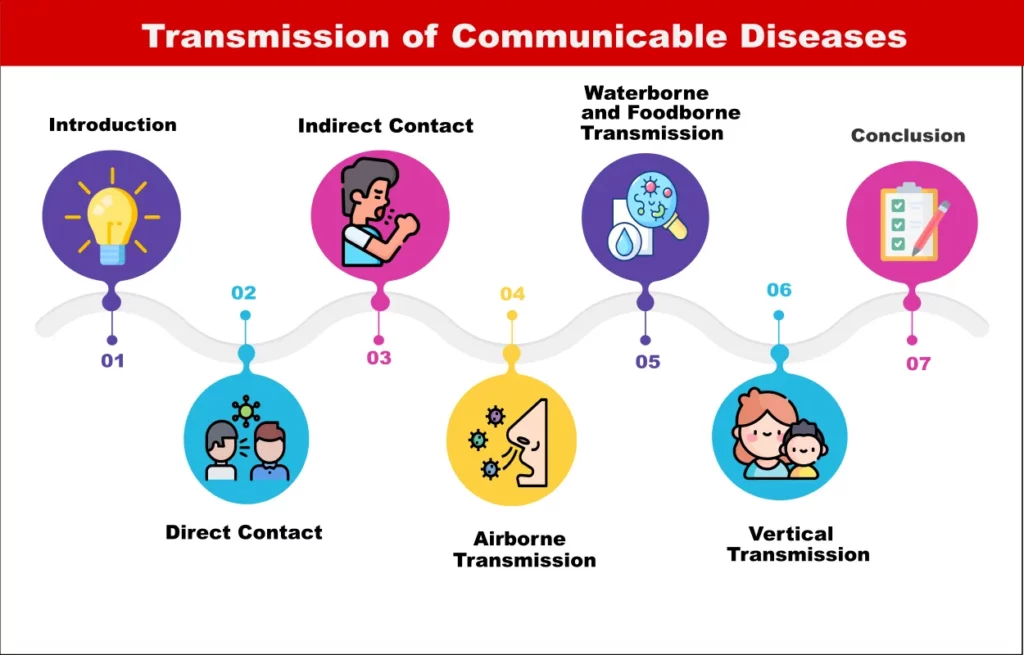
TYPES OF TRANSMISSION
There are several types of transmission for communicable diseases, each based on how the disease-causing pathogen spreads from one host to another. Here are the main types:
1. DIRECT TRANSMISSION
The Communicable Disease happens when a virus is directly transferred from an infected person or animal to a healthy person. It consists of:
Person-to-person interaction:
Handshakes and hugs are examples of physical touch. Examples include skin diseases, herpes, and HIV.
Mother-to-child transmission:
During pregnancy, childbirth, or breastfeeding, an infected mother may transmit her communicable disease to her unborn child. Hepatitis B and HIV are two examples.
2. INDIRECT TRANSMISSION
The Communicable disease spreads through an intermediary, like contaminated surfaces or items, in this kind of transmission. This can occur by:
Fomites:
Infected items or surfaces that an uninfected individual comes into contact with. Examples include the flu, the common cold, and gastrointestinal illnesses brought on by bacteria such as E. coli.
Airborne Transmission:
When infections travel through the atmosphere as microscopic particles or droplets that other people may inhale Long distances and frequently poorly ventilated environments might cause this. Measles, chickenpox, and tuberculosis are a few examples.
3. VECTOR-BORNE TRANSMISSION
In this instance, the infection is spread from one host to another by a living thing, typically an animal or insect. The Communicable disease is frequently spread by the vectors without any personal injury. Typical instances include:
- Lyme disease and Rocky Mountain spotted fever-carrying ticks.
- Mosquitoes that spread dengue, malaria, Zika virus, and yellow fever.
- The spread of Communicable disease by fleas.
4. DROPLET TRANSMISSION
When an infected person coughs, sneezes, talks, or breathes, pathogens are released from their respiratory tract as droplets. When these droplets land on surfaces or are inhaled, they can spread to other people. Among the examples are:
- Influenza (flu)
- COVID-19
- Common cold
5. AIRBORNE TRANSMISSION
Comparable to droplet Communicable Disease transmission, but with much smaller germs that can travel farther and stay suspended in the air for longer. Among the examples are:
- Tuberculosis (TB)
- Measles
- Chickenpox
6. FECAL-ORAL TRANSMISSION
This kind of Communicable Disease transmission happens when fecal pathogens are consumed by the body, usually through tainted food, water, or surfaces. Typical instances consist of:
- Cholera
- Hepatitis A
- Norovirus
7. ZOONOTIC TRANSMISSION
8. VERTICAL TRANSMISSION
The Communicable Disease happens when a parent’s illness is passed on to their child, typically during pregnancy, childbirth, or nursing. Among the examples are:
- HIV
- Rubella
- Syphilis
9. PARENTERAL TRANSMISSION
- Blood or Needles: Infected people transmit infections when their blood enters another person’s bloodstream, typically through needles or other sharp objects. Additionally, blood transfusions or organ transplants can also facilitate transmission. For instance, HIV, hepatitis B and C, and malaria in certain regions are examples of such infections.

HOW PERSON SUFFER FROM IT ?
When a person contracts a pathogen—such as a virus, bacteria, fungus, or parasite—that can be spread from another person, animal, or environment, they are said to have a communicable disease. The pathogen type, the patient’s immune system, and the disease’s characteristics all affect how severe and what symptoms the patient experiences. A person usually contracts a communicable disease in the following ways:
EXPOSURE TO THE PATHOGEN
A person can become infected through one of the various means of transmission:
- Contaminated food or water, which can introduce pathogens into the digestive system (e.g., cholera, salmonella).
DEVELOPMENT OF SYMPTOMS
Symptom Development The pathogen causes a variety of symptoms as it spreads throughout the body, depending on the organ systems and type of infection. These symptoms include:
- Fever: The body raises its temperature to help fight off infection.
- Fatigue: The body uses energy to fight off the disease, causing tiredness.
- Pain: Infection can cause inflammation and pain in affected areas.
- Cough, sore throat, or runny nose: Respiratory infections like the flu or COVID-19 can cause symptoms in the respiratory system.
- Digestive symptoms: Gastroenteritis, such as nausea, vomiting, diarrhea, or cramping in the stomach.
- Rashes or sores: Skin infections, like chickenpox or measles, may leave visible marks on the skin.
RECUPERATION OR SEVERE DISEASE
The patient may need medical treatment, such as antibiotics for bacterial infections or antiviral drugs for viral disorders, or they may heal on their own when the immune system gets rid of the infection. Certain infectious infections can cause severe illness or even death in extreme circumstances if they are not properly treated.
The term “recuperation” refers to the process of recovering or regaining strength and health after an illness or injury. It involves rest, treatment, and the gradual return to normal functioning.On the other hand, “severe disease” refers to a condition or illness that is intense or extreme in nature.
INCUBATION PERIOD
After the pathogen enters the body, it typically goes through an incubation period, which is the time between exposure and the appearance of symptoms. This period can vary from a few hours to several weeks, depending on the disease. During this period, the person may not feel sick but can still be contagious.
THE IMMUNE REACTION
By creating antibodies, triggering white blood cells, and starting other defense mechanisms, the body’s immune system fights the infection. The pathogen, however, will determine whether the immune system is able to eradicate the infection or becomes overloaded, resulting in more serious symptoms or problems.
DISEASE TRANSMISSION
Even though a person is exhibiting symptoms, they are frequently contagious and have the ability to infect others. Direct contact, breathing droplets, or other means of transmission, like coming into contact with contaminated surfaces, can all cause this.
CONSEQUENCES
In certain situations, improper treatment or a compromised immune system might result in consequences from a communicable disease. These issues could consist of:
- Pneumonia: A serious lung infection frequently linked to respiratory illnesses such as COVID-19 or the flu.
- Dehydration: Infections like cholera or norovirus can cause severe vomiting or diarrhea.
- Chronic disease: Long-term health issues can result from certain infections, such HIV.
- Organ damage: Some infections have the ability to harm important organs, such the kidneys or liver (in the case of hepatitis).
NAME & INTRODUCTION OF COMMUNICABLE DISEASE
1.Malaria
Malaria is a life-threatening infectious disease caused by parasites transmitted to humans through the bites of infected female mosquitoes.
2.Influenza (Flu)
Influenza, also referred to as the flu, is a respiratory disease that is spread by influenza viruses.
3.Tuberculosis (TB)
Tuberculosis is a bacterial infection that primarily affects the lungs and spreads through the air when an infected person coughs or sneezes.
4.COVID-19
COVID-19 is a respiratory illness caused by the SARS-CoV-2 virus, primarily transmitted through respiratory droplets.
5.Measles
Measles is a highly contagious viral infection characterized by symptoms such as a high fever, cough, runny nose, and a distinctive red rash.
6.HIV/AIDS
The virus known as HIV (Human Immunodeficiency Virus) targets the immune system, impairing the body’s capacity to fight against infections. HIV can cause AIDS (Acquired Immunodeficiency Syndrome), a disorder in which the immune system is seriously weakened, if treatment is not received.
7.Hepatitis B
Hepatitis B is a viral infection that affects the liver, causing symptoms like jaundice, fatigue, and abdominal pain.
8.Chickenpox
Chickenpox is a highly contagious viral infection that causes an itchy skin rash, fever, and general discomfort.
9.Cholera
Cholera is an acute diarrheal infection caused by ingesting contaminated food or water, leading to severe dehydration.
10.Whooping cough
The Bordetella pertussis bacteria is the cause of the highly contagious respiratory illness known as whooping cough.
11.Fever from dengue
The virus that causes dengue fever is spread by mosquitoes, namely the Aedes aegypti species.
12.Zika Virus
Zika virus is primarily spread by Aedes mosquitoes and can lead to symptoms such as fever, rash, and joint pain.
13.Mumps
Mumps is a viral infection caused by the mumps virus, known for causing swelling of the salivary glands.
14.Tetanus
Tetanus is a bacterial infection caused by Clostridium tetani, often entering the body through deep cuts or puncture wounds.
15.Scarlet Fever
Scarlet fever is a bacterial infection caused by Streptococcus pyogenes, which produces a toxin leading to a distinctive red rash.
16.Norovirus
The highly contagious norovirus virus causes gastroenteritis, which manifests as cramping in the stomach, diarrhea, and vomiting.
17.Syphilis
Treponema pallidum is the bacterium that causes syphilis, an infection spread through sexual contact.
18.Leprosy (Hansen’s Disease)
Leprosy is a chronic infectious disease caused by Mycobacterium leprae that affects the skin, nerves, and upper respiratory tract.
19.Rubella (German Measles)
Rubella is a viral infection characterized by a mild fever and a rash, typically affecting children.
20.Rabies
Rabies is a viral infection that affects the central nervous system, transmitted through the bite of an infected animal. Top of FormBottom of Form

EXAMINING CASES
CASE STUDY 1: HIV & EXPERIENCE OF MR. AJAY
Five years ago, Mr. Ajay, a 35-year-old man, received an HIV diagnosis. He had been using intravenous drugs for more than ten years, and during that time, he shared needles, which is how HIV is most likely to spread. Significant changes started to occur after 18 months of intense counseling, support for medication adherence, and psychiatric therapy. Mr. Ajay’s example highlights the difficulty of controlling HIV in people who have a history of substance use disorder. He was able to overcome major obstacles and reach recovery with a mix of ART, addiction treatment, psychiatric care, and psychological support.His accomplishments showcase the importance of a well-rounded approach to rehabilitation. This approach considers both the psychological and medical aspects of addictionIt also addresses the challenges faced by individuals living with HIV. By integrating these elements, rehabilitation becomes more effective and holistic.
CASE STUDY 2 : AIDS & FIGHT OF MR. MUKESH
Five years ago, Mr. Mukesh, a 40-year-old man, received an AIDS diagnosis. He has a lengthy history of intravenous drug use (IVDU) spanning more than 15 years, during which time he shared needles often, likely contributing to the spread of AIDS. In addition, he has a history of mental health issues and alcohol consumption. The story of Mr. Mukesh demonstrates the serious effects of substance abuse on AIDS care. His continued addiction mental health problems, and poor treatment adherence hindered his recovery even after getting ART and other medical measures. In order to improve results, his story highlights the necessity of managing HIV in people with drug abuse disorders through a comprehensive, multidisciplinary strategy that combines addiction treatment, mental health assistance, and medical care. Unfortunately, Mr. MUKESH was unable to recover from AIDS if these important issues were not addressed.
SIGN & SYMPTOMS OF AN INFECTION :
The signs and symptoms of communicable diseases can vary depending on the specific illness, but in general, they may include:
Common Signs and Symptoms:
Fever: A common symptom indicating infection or inflammation.
Cough: Often present in respiratory infections like the flu, tuberculosis, or COVID-19.
Fatigue: General tiredness or lack of energy is a frequent symptom of many communicable diseases.
Body Aches: Muscle or joint pain, common in flu and viral infections.
Rashes: Skin rashes can appear in diseases like measles, chickenpox, and rubella.
Sore Throat: A common symptom in respiratory infections such as streptococcal throat infection and viral upper respiratory infections.
Diarrhea and Vomiting: Can occur in gastrointestinal infections like cholera, norovirus, or food poisoning.
Headache: Can occur in diseases like meningitis, malaria, or flu.
Chills: Often experienced along with fever in infections like malaria.
Breathing Problems: Difficulty breathing or shortness of breath, seen in diseases like pneumonia or COVID-19.
HOW IT RELATE TO ADDICTION ?
There are several connections between communicable diseases and addiction, particularly when taking into account the circumstances and behavior of those who are battling addictionThis is how they are related:
1.A greater susceptibility to infection
The immune systems of those who suffer from addiction, especially to substances like alcohol, opioids, or intravenous narcotics, may be compromised. They are therefore more vulnerable to catching infectious infections.
2.Infectious Disease-Spreading Behaviors
Risky actions brought on by addiction can directly aid in the spread of infectious diseases. For instance:
Cohabitation and homelessness: Substance abuse can result in living in cramped quarters where illnesses like the flu, TB, and other respiratory infections can more readily spread.
3.Health and Hygiene Compromise
Addictionespecially to drugs or alcohol that affect mental or physical functioning, can cause people to neglect their personal hygiene or seek medical attention. This may lead to:
A higher chance of infections (such as pneumonia or skin diseases).
Inadequate hydration and nourishment, which impair immunity and reduce the body’s capacity to fight off infections.
4.Treatment Obstacles
Accessing healthcare or programs for preventing communicable diseases may be difficult for people who are addicted. Among these obstacles are:
Stigma: People may be deterred from seeking medical attention for infectious diseases or addiction therapy due to the stigma attached to addiction.
Limited access to healthcare: Addiction can result in social isolation or financial instability, which can both limit access to healthcare services like immunizations, infectious disease treatment, and preventative care.
5.Mental health disorders that co-occur
Addicts frequently suffer from mental health conditions such trauma, anxiety, or depression. Adhering to preventive measures that lower the risk of communicable diseases can be more challenging for people with certain co-occurring ailments.
HOW COMMUNICABLE DISEASE AFFECTS IMMUNITY
Depending on the pathogen type (bacteria, viruses, fungi, or parasites) and the body’s reaction to the infection, infectious diseases can have a substantial impact on the immune system in a number of ways. Immunity can be affected by communicable diseases in the following ways:
1. Impact on Immune Cells Directly
The immune system’s cells and organs are directly impacted by some communicable diseases. They specifically target and harm CD4 T cells, which are immunological cells that are essential in the fight against infections. where the body is susceptible to opportunistic infections and malignancies due to a severely weakened immune system.
2. Immune System Overload
The immune system may become overloaded by some infectious illnesses, resulting in inflammation or excessive immunological reactions. Strong inflammation brought on by the flu virus can help the body fight the virus, but occasionally this reaction gets out of control and damages bodily tissues. In extreme situations, it may lead to consequences that put further stress on the immune system.
3. Immunosuppression
Certain infections deliberately weaken the immune system to help the pathogen survive and proliferate. These viruses have the ability to elude the immune system and result in persistent infections, which can induce cirrhosis and liver damage. The body’s capacity to develop a successful defense against other illnesses may also be weakened by persistent infections. Communicable Disease can weaken the immune system, especially in those who have had infections frequently, leaving them more vulnerable to other illnesses.
4. Immune Evasion Strategies
Pathogens have evolved a number of defense mechanisms to evade immune system recognition and elimination. create latency in nerve cells to prevent the immune system from detecting them. The virus may not be active during dormant periods, but it may reawaken when the immune system is suppressed, as it is during stress or Communicable disease.
5. Secondary Infections
The immune system is weakened by certain communicable diseases, making it easier for additional infections to occur. Common colds and other Communicable diseases can impair immunity or harm respiratory tissues, which facilitates the development of bacterial infections like pneumonia.
6. Vaccination and Immunity
Through vaccination, the immune system can form a memory of the pathogen in response to some communicable diseases. In order to trigger the production of antibodies and immune cells that will identify and fight the pathogen should it reappear, vaccines expose the immune system to a weakened or inactivated form of the pathogen. However, in those with compromised immune systems as a result of disease or underlying disorders, the immunological response to vaccinations may occasionally be compromised.
7. Chronic Inflammation
Persistent low-level inflammation can result from certain communicable diseases, particularly those that induce chronic infection. Over time, this persistent inflammation can weaken the immune system, reducing its ability to fight off infections or other health risks.
WHAT SHOULD PERSON DO TO PREVENT FROM THESE DISEASE
Personal hygiene habits, immunizations, healthy lifestyle choices, and abstaining from behaviors that raise the risk of infection are all part of the prevention of communicable illnesses. A person can lower their risk of catching or transmitting infectious diseases by doing the following crucial actions:
1. MAINTAIN PROPER HYGIENE
- Handwashing: Before eating, after coughing or sneezing, and especially after using the restroom, wash your hands well with soap and water. This aids in eliminating germs and stops illnesses from spreading.
- Use Hand Sanitizer: To eradicate germs, use an alcohol-based hand sanitizer in the absence of soap and water.
- Cover Your Mouth and Nose: To stop respiratory infections from spreading, always cover your mouth and nose when you cough or sneeze with a tissue or your elbow.
- Clean and Disinfect Surfaces: Regularly clean and disinfect frequently touched surfaces, like doorknobs, light switches, and phones, especially during cold and flu season.
2. VACCINATION
- Vaccinate: One of the best defenses against a variety of infectious diseases, including the flu, hepatitis B, measles, rubella, and pneumonia, is vaccination. Follow your doctor’s advice and stay current on your children’s and your own required vaccines.
- COVID-19 Vaccine: To lower the risk of serious illness, hospitalization, and virus transmission, get the COVID-19 vaccine if you are eligible.
3. AVOID SHARING PERSONAL ITEMS
- Avoid Sharing Needles or Razors: Needles, syringes, and other objects that may harbor bloodborne infections such as HIV and hepatitis B and C should never be shared. Make sure the needles are sterile and clean before utilizing them for medical purposes.
- Refrain from sharing personal hygiene items and towels: It’s crucial to avoid sharing items that can transfer illnesses, such as towels, toothbrushes, and razors.
4. MAINTAIN A HEALTHY IMMUNE SYSTEM
- Consume a Balanced Diet: A diet high in fruits, vegetables, whole grains, lean meats, and healthy fats helps the body fight off infections and boosts immunity.
- Get Regular Exercise: Engaging in moderate physical activity can strengthen the immune system and lower the chance of developing chronic illnesses.
- Stay Hydrated: Drinking plenty of water helps the body function properly and supports overall health.
- Get Adequate Sleep: Sleep is vital for immune function. Aim for 7–9 hours of decent sleep each night.
- Control Stress: Prolonged stress impairs immunity. Engage in relaxing activities, meditation, or deep breathing as stress-reduction strategies.
5. AVOID EXPOSURE TO ENVIRONMENTAL HAZARDS
- Don’t Smoke: Smoking impairs immunity and makes one more vulnerable to respiratory illnesses like TB and pneumonia. Giving up smoking strengthens the immune system as a whole.
- Limit Alcohol Use: Drinking too much alcohol impairs immunity and raises the chance of infection. Maintaining excellent health can be achieved by refraining or drinking in moderation.
6. AVOID CLOSE CONTACT WITH SICK PEOPLE
- Avoid Crowded Places: During flu season or outbreaks of contagious diseases (like COVID-19), stay away from crowded places or gatherings to limit your exposure to potential infections.
- Stay at Home When Sick: If you’re feeling ill, especially if you have symptoms of a contagious illness (such as fever, cough), stay at home to avoid spreading the disease to others.
7. USE INSECT PROTECTION
Insect repellents : To protect against diseases like dengue, malaria, and the Zika virus that are spread by mosquitoes. Wear protective clothing, such as long sleeves, pants, and socks, when in areas where mosquito activity is high.
Use bed nets: In areas where mosquito-borne illnesses are prevalent, sleeping under a bed net treated with insecticide can help prevent mosquito bites during the night.
8. PRACTICE SAFE FOOD HANDLING
- Cook Food Properly: Make sure that meat, poultry, eggs, and seafood are cooked to the recommended internal temperatures to kill harmful bacteria and viruses.
- Store Food Properly: Keep perishable food in the refrigerator or freezer to prevent the growth of bacteria and viruses.
- Wash your hands before cooking: Always wash your hands before preparing or eating food to avoid contamination.
9. SEEK MEDICAL CARE EARLY
- Consult a Physician for Preventive Care: Early intervention, screenings, and routine health examinations can all aid in identifying and stopping the spread of illnesses.
- Adhere to Treatment Plans: To guarantee that an infection is appropriately managed and to prevent the infection from spreading to others, if you have been diagnosed with a communicable disease, adhere to your doctor’s treatment plan.
10. ADOPT SAFE TRAVEL PRACTICES
- Learn About Travel Health Risks: Consult a healthcare professional about any required vaccinations or drugs prior to travel, particularly to regions with increased illness risks (such as malaria or tuberculosis)
- Steer Clear of Contaminated Water: Steer clear of untreated water and raw food that can be contaminated when visiting areas with poor hygiene.
11. COVER COUGHS AND SNEEZES:
- Use a tissue or the inside of your elbow to cover your mouth and nose when coughing or sneezing.
- Dispose of tissues immediately and wash your hands afterward.
- Always try to cough or sneeze into a tissue. After using the tissue, dispose of it immediately in a trash bin.
- Wash your hands right after disposing of the tissue.
RISK & DEFENSE FROM INFECTION : “ HYGINE ”
Hygiene plays a critical role in protecting the body from infections. By maintaining good hygiene practices, you reduce the risk of exposure to harmful pathogens like bacteria, viruses, and fungi that can cause infections. Here’s how hygiene contributes to defense against infections:
1. HAND HYGIENE
- Washing Hands Regularly: One of the most effective ways to prevent the spread of infections. Washing hands with soap and water for at least 20 seconds, especially after using the bathroom, before eating, and after touching potentially contaminated surfaces, reduces the likelihood of infection transmission.
- Using Hand Sanitizer: If soap and water are unavailable, hand sanitizers with at least 60% alcohol can kill many germs and viruses.
2. PERSONAL HYGIENE
- Showering or Bathing Regularly: Keeping the skin clean prevents the buildup of sweat, dirt, and bacteria that could lead to infections, such as skin irritations or fungal infections.
- Brushing Teeth: Maintaining oral hygiene by brushing teeth twice daily and flossing helps prevent dental infections and gum disease.
- Nail Hygiene: Keeping nails trimmed and clean helps prevent the buildup of dirt and bacteria under the nails, which can lead to infections.
3. PROPER USE OF TOILETS AND SANITATION
- Using Toilets Safely: Always use clean toilets and wash hands immediately afterward to avoid cross-contamination with harmful pathogens.
- Safe Disposal of Waste: Proper disposal of waste (such as tissues or sanitary products) ensures pathogens don’t spread in the environment.
4. FOOD AND WATER HYGIENE
- Washing Fruits and Vegetables: Before eating, always wash produce to remove harmful bacteria, pesticides, and dirt.
- Safe Food Handling: Proper cooking and storing food at the right temperature can prevent foodborne illnesses.
- Clean Drinking Water: Ensuring access to clean, safe drinking water is vital for avoiding infections from waterborne pathogens.
5. ENVIRONMENTAL HYGIENE
- Cleaning Surfaces: Regular cleaning of frequently touched surfaces (e.g., doorknobs, countertops, phones) reduces the likelihood of viral and bacterial spread.
- Air Quality: Good ventilation helps reduce the accumulation of airborne pathogens and allergens that can cause respiratory infections.
6. PERSONAL PROTECTIVE MEASURES
- Wearing Masks and Gloves: In certain situations (e.g., during a flu outbreak or when handling potentially contaminated items), wearing protective gear can help limit the spread of infections.
- Social Distancing: Limiting close contact with sick individuals, especially during flu seasons or pandemics, helps to minimize the spread of infectious diseases.
- Limit touching your eyes, nose, and mouth to reduce the chance of transferring germs from surfaces to your body.
- Rest and recover: If you’re feeling unwell, avoid going to work, school, or public places to prevent the spread of infection.
GOVERNMENT STRATEGIES TO REGULATE COMMUNICABLE DISEASE
Governments play a critical role in preventing and controlling the spread of communicable diseases. Effective strategies involve a combination of public health policies, education, healthcare infrastructure, and international collaboration. Here are the key strategies that governments typically use to regulate communicable diseases:
1. SURVEILLANCE AND MONITORING
- Disease Surveillance Systems: Governments establish systems to monitor the incidence of communicable diseases in real-time. This helps in early detection, tracking outbreaks, and understanding patterns of disease spread.
- Reporting Requirements: Health facilities and healthcare professionals are often required to report cases of certain communicable diseases to public health authorities, enabling quick responses to outbreaks.
2. VACCINATION PROGRAMS
- Immunization Campaigns: Vaccination is one of the most effective tools for preventing the spread of communicable diseases. Governments often run national vaccination programs targeting diseases such as polio, measles, hepatitis, and influenza.
- Mandating Vaccination: In some cases, vaccines may be mandatory for certain groups, such as healthcare workers or schoolchildren, to prevent outbreaks and protect public health.
3. PUBLIC HEALTH EDUCATION AND AWARENESS
- Campaigns and Information: Governments often run public health education campaigns to inform citizens about preventive measures (e.g., hand hygiene, safe food handling, and vaccination).
- Targeted Education: Specific campaigns may focus on high-risk populations, such as those living in overcrowded areas or healthcare workers who may be more vulnerable to certain diseases.
4. HEALTHCARE INFRASTRUCTURE AND ACCESS
- Strengthening Healthcare Systems: Governments invest in healthcare facilities, personnel, and medical equipment to ensure the ability to diagnose, treat, and isolate communicable diseases.
- Access to Care: Ensuring that all citizens have access to healthcare services, including diagnostic testing and treatment for infectious diseases, is a crucial part of preventing the spread of disease.
5. QUARANTINE AND ISOLATION MEASURES
- Quarantine Regulations: During outbreaks of highly contagious diseases, governments may implement quarantine measures to separate infected individuals from healthy populations.
- Isolation Facilities: Establishing isolation centers for those diagnosed with infectious diseases helps prevent the spread to others.
6. SOCIOCULTURAL AND BEHAVIORAL INTERVENTIONS
- Targeted Interventions for High-Risk Groups: Governments may implement strategies tailored to high-risk communities (e.g., urban slums, refugee camps) that include education, preventive measures, and vaccination campaigns.
- Behavioral Change Programs: Encouraging safe practices such as condom use to prevent HIV/AIDS or safe water practices to prevent waterborne diseases is an important part of regulation.
6. TRAVEL AND BORDER CONTROL
- Travel Restrictions: In cases of outbreaks (such as COVID-19), governments may implement travel restrictions or advisories to prevent the spread of diseases across borders.
- Health Screening at Borders: Screening travelers for symptoms of infectious diseases at airports, seaports, and land borders can help detect and control the movement of contagious individuals.
7. PUBLIC HEALTH LEGISLATION AND REGULATIONS
- Mandatory Reporting Laws: Governments may require the reporting of specific diseases by healthcare providers to public health authorities to enable prompt action.
- Control of Vector-Borne Diseases: Laws and regulations governing the control of vectors (such as mosquitoes) that transmit diseases like malaria, dengue, and Zika are crucial for limiting the spread of such diseases.
- Infection Control in Healthcare Settings: Regulations that mandate infection control practices in hospitals and clinics help reduce the risk of hospital-acquired infections.
8. COLLABORATION AND COORDINATION
- International Collaboration: Governments often collaborate with international organizations such as the World Health Organization (WHO) to share information, resources, and expertise in managing outbreaks and disease prevention on a global scale.
- Coordination Between Sectors: Effective regulation of communicable diseases often requires collaboration between various government sectors (e.g., health, education, transportation, agriculture) to address the multiple determinants of disease spread.
9. RESEARCH AND DEVELOPMENT
- Funding Research: Governments fund research to develop new vaccines, diagnostic tools, and treatments for communicable diseases. This helps in the long-term fight against infections that may not yet have effective treatments or prevention methods.
- Support for Public Health Studies: Governments also support studies on social determinants of health, patterns of disease transmission, and strategies for improving public health interventions.
10. EMERGENCY PREPAREDNESS AND RESPONSE
- Preparedness Plans: Governments develop national and regional emergency preparedness plans to respond to communicable disease outbreaks, ensuring a coordinated, efficient response when new or re-emerging infectious diseases occur.
- Stockpiling Essential Supplies: Governments stockpile medicines, vaccines, personal protective equipment (PPE), and other essential supplies for rapid deployment during disease outbreaks.
13. INTERNATIONAL COLLABORATION
- Cross-border disease control: Working with international organizations like the World Health Organization (WHO) to prevent the global spread of diseases.
- Information sharing: Governments collaborate on sharing disease data and resources for combating pandemics.
QUICK MEDICATION FOR INFECTION
When it comes to infections, quick, effective, and easily available medications can significantly reduce the severity and duration of illness. However, the type of medication needed depends on the type of infection (bacterial, viral, fungal, etc.). Below are some commonly used medications for various infections that are generally accessible:
1. Antibiotics for Bacterial Infections
- Amoxicillin: Commonly used to treat a variety of bacterial infections such as ear infections, respiratory infections, and urinary tract infections (UTIs).
- Azithromycin: Often prescribed for respiratory infections, pneumonia, and sexually transmitted infections (STIs).
- Doxycycline: Used for a range of bacterial infections including respiratory tract infections, skin infections, and some STIs (e.g., chlamydia).
2. Antivirals for Viral Infections
- Oseltamivir (Tamiflu): This antiviral medication is used to treat influenza (flu) and can reduce the duration of symptoms if taken within 48 hours of onset.
- Acyclovir: Used for herpes simplex virus (HSV) infections, such as cold sores, genital herpes, or shingles.
3.Antifungals for Fungal Infections
- Clotrimazole: A topical antifungal cream commonly used for skin infections like athlete’s foot, ringworm, and yeast infections (vaginal or oral).
- Fluconazole: An oral antifungal medication often used for systemic infections, including candidiasis (yeast infections) and certain types of fungal pneumonia.
4.Over-the-Counter (OTC) Medications
- Paracetamol (Acetaminophen): While not an antibiotic or antiviral, this pain reliever and fever reducer is commonly used to manage symptoms of many infections like the flu, cold, or viral respiratory infections.
- Ibuprofen: Another pain reliever and anti-inflammatory drug that helps with fever and pain associated with infections.
5.Topical Antibiotics for Skin Infections
- Neosporin (Triple Antibiotic Ointment): Contains neomycin, polymyxin B, and bacitracin, which help prevent infection in minor cuts, scrapes, and burns.
- Hydrocortisone Cream: While primarily an anti-inflammatory, it can help reduce itching and inflammation associated with mild skin infections, though it shouldn’t be used for serious bacterial infections.
6.Probiotics for Gut Health
- Lactobacillus: Probiotic supplements can help restore healthy gut bacteria, particularly after taking antibiotics, which can disrupt the balance of microorganisms and increase the risk of secondary infections like Clostridium difficile (C. diff).
7. Antiseptics for Wound Care
- Hydrogen Peroxide: Commonly used to clean wounds and prevent infection.
- Iodine-based solutions (Betadine): Effective at cleaning and disinfecting minor cuts, abrasions, and burns to prevent infection.